All About Clotting Disorders
How Blood Clotting Works
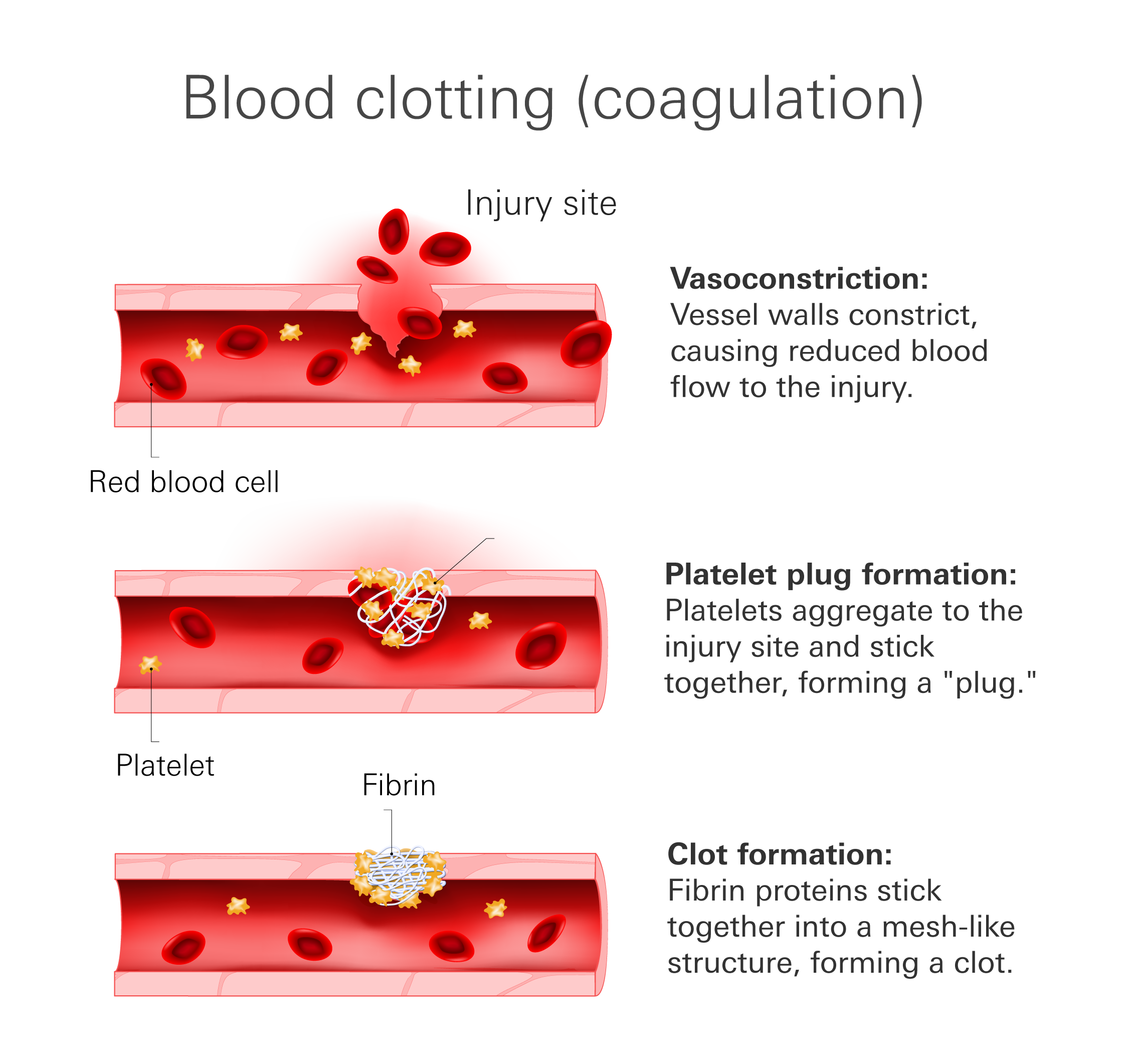
When we get a cut or scrape, our blood vessels are damaged, causing blood to leak out. This activates platelets, small cell fragments in the blood, which come together to form a sticky plug that stops the bleeding.
However, platelets alone are not enough to stop bleeding. A clot is needed at the site of injury.
The clotting process relies on substances known as clotting factors, which are numbered I to XIII in Roman numerals. These factors interact with each other in a sequence called the clotting cascade. Ultimately, fibrinogen, a soluble protein in the blood, is converted into fibrin, an insoluble protein. The fibrin molecules then bind together, creating a clot.
Once the clot forms, it acts as a natural barrier, protecting our bodies from too much blood loss. This triggers the healing process, where new cells grow, and the wound gradually heals.
Dangerous Blood Clots
Blood clotting is a vital process that helps prevent excessive bleeding when we get injured. However, sometimes this blood clotting occurs when and/or where it isn’t supposed to. Other times, the clot forms properly, but then does not dissolve when it should.
This is dangerous because an unwanted or undissolved blood clot can block oxygen and nutrients from being delivered to your tissues. This can result in tissue death where the blood does not reach.
Common blood clots are typically characterized by their location, and include:
- Myocardial infarctions (MI)
A myocardial infarction, or “heart attack”, is a condition often caused by a blood clot blocking blood flow to the heart. - Ischemic stroke (IS)
An ischemic stroke is a condition caused by a blockage of blood flow to part of the brain. - Pulmonary embolism (PE)
A pulmonary embolism is a blockage in the blood vessels of your lungs, often caused by a clot that has broken off elsewhere in the body and lodged itself in your lungs. - Deep vein thrombosis (DVT)
A DVT is a clot or “thrombosis” that occurs in one of the deep veins. This most often includes veins in your legs, pelvis, or sometimes arms.
Clotting Disorders
There are a number of conditions in which you are at a greater risk of developing a blood clot. These conditions can be genetic (you are born with it) or acquired (you develop it later in life). Some of the more common genetic clotting disorders include Factor V Leiden and Prothrombin 20210A mutation. Acquired conditions include antiphospholipid syndrome and disseminated intravascular coagulation.
Factor V Leiden
Factor V Leiden (FVL) is a genetic mutation of the clotting factor V in the blood and a common cause of thrombophilia, a tendency to develop abnormal blood clots. Caucasians from Europe and North America have a higher likelihood of the condition. Roughly 5/100 of these individuals inherit one copy of this mutation, while 1/5,000 inherit two copies.
Factor V helps form a stable blood clot during clotting process. However, in people with Factor V Leiden, a specific mutation in the F5 gene makes the factor V protein more resistant to degradation by a protein called activated protein C (APC). As a result, factor V Leiden increases the risk of abnormal blood clot formation, primarily in the veins.
Individuals with Factor V Leiden have an increased risk of developing deep vein thrombosis (DVT), which is the formation of blood clots in the deep veins, typically in the legs. These clots can sometimes break free and travel to the lungs, causing a potentially life-threatening condition called pulmonary embolism (PE).
This clot risk is even more increased in certain situations, such as during pregnancy. There is also thought to be an increased risk of recurrent miscarriages, and other pregnancy-related conditions such as preeclampsia.
Most individuals with this mutation will not experience any unwanted clots, though it is important to be aware of this increased risk.
Diagnosis
Your doctor may consider genetic testing for Factor V Laiden in the following situations:
- Personal or family history of blood clots: If you or a close family member have a history of unexplained blood clots, particularly deep vein thrombosis (DVT) or pulmonary embolism (PE).
- Recurrent or unusual blood clots: If you have experienced recurrent or unusual blood clots at a young age, without clear risk factors such as surgery, trauma, or prolonged immobility, genetic testing may be recommended.
- Multiple unexplained VTE/PEs
- VTE (venous thromboembolism) at a young age (<50 years old)
- Unexplained arterial blood clot
- Atypical sites of VTE (ovarian vein, renal vein)
- VTE during hospitalization while on anti-clotting medication
Treatment
Most poeple with FVL do not form abnormal clost and do not require any specific treatment. If a clot does form, it is treated in the same way as any other PE or DVT.
In general, management of FVL are most focused on prevention. Prevention of clots includes reducing your risk on a general basis, such as smoking cessation, increased exercise, caution with estrogen-containing medications. This also includes taking extra precautions when in situations that put you at greater risk of a clot, including surgery and long-haul flights.
These preventative measures could include any combination of:
- A short course of a blood thinner (anticoagulant) medication
- Compression socks
- Avoiding sitting for extended periods of time
Prothrombin Gene Mutation (G20210A)
Prothrombin Gene Mutation (PGM), also known as a Factor II Mutation, is another genetic clotting disorder. Slightly more common than FVL, Prothrombin Gene Mutation affects roughly 1 in 50 Caucasians. Depending on if one or both of your parent’s genes are affected, your chance of developing this condition can be anywhere from 25-100%.
Prothrombin is a precursor protein that converts to thrombin, an enzyme that promotes blood clot formation. Individuals with the prothrombin gene mutation have an alteration in the gene sequence that leads to increased production of prothrombin, resulting in a higher concentration of thrombin in the blood.
Thrombin contains both pro- and anti-clotting effects, which plays a role in ensuring clotting remains in balance between enough clotting, but not too much.
A higher concentration of thrombin results in a higher tendency to form blood clots. In particular, the prothrombin gene mutation (PGM) is associated with a 2-4 times higher risk of developing a venous thromboembolism (VTE).
Diagnosis
There are no symptoms of PGM. It is typically suspected through a knowledge of a family history. Otherwise, it can sometimes be suspected if a blood clot occurs under suspicious circumstances.
- Having multiple unprovoked blood clots on different occasions
- Having a blood clot at a young age
If you are suspected of having a clotting disorder, you will most likely undergo genetic testing to see if there is a mutation to the G20210A gene. Once diagnosed, your healthcare provider will discuss what this mutation means for you and your health.
Treatment
The main treatment for PGM is to prevent blood clots through lifestyle changes.
- Quitting smoking
- Avoiding estrogen-based birth controls
- Avoiding sitting for extended periods of time
Antiphospholipid Syndrome
Antiphospholipid syndrome (APS) is an auto-immune condition, meaning your immune system begins to mistakenly attack your body. Under normal circumstances, the immune system creates antibodies against harmful foreign materials such as viruses and bacteria. In the case of APS, your immune system makes antibodies against phospholipids, which are fat molecules that flow through your blood.
The main feature of APS is an increased tendency to develop blood clots, particularly in the veins (venous thrombosis) or arteries (arterial thrombosis). This can lead to various health problems, depending on the location and size of the blood clot.
- Venous thromboembolism (VTE)
- Myocardial infarction (MI)
- Ischemic stroke (IS)
- Recurrent miscarriages and/or premature births
Causes
While the exact cause of APS is unknown, there are two classifications:
- Primary APS occurs without a known explanation. This is the most common.
- Secondary APS occurs as a result of another autoimmune condition, such as lupus or rheumatoid arthritis.
In either situation, there are factors that increase your risk of developing APS.
- Female sex
- Certain genetic mutations
- Certain infections, such as HIV
- Various medications, such as procainamide or quinidine
Diagnosis
While rare, some people with APS experience symptoms including:
- Chronic headaches
- Rash
- Abnormal lab values (low platelets, signs of heart disease)
Most people with APS have no symptoms. It is only suspected following suspicious clots or recurrent miscarriages. Once suspected, the condition is diagnosed by testing the blood for the presence of anti-phospholipid antibodies. This bloodwork will also allow your healthcare provider to rule out other conditions, such as other clotting disorders.
Treatment
APS can not be cured, and treatment targets prevention of APS-related events. This often involves the use of blood-thinning medications, such as low-dose aspirin or anticoagulants (e.g., warfarin or heparin), to reduce the risk of clot formation. It is particularly important if you are pregnant or planning to become pregnant. Taking pregnancy-safe blood thinners is extremely important during pregnancy with APS in order to decrease the risk of miscarriage and other pregnancy-related conditions.
Disseminated Intravascular Coagulation
Disseminated intravascular coagulation (DIC) is a very serious condition and characterized by the simultaneous activation of both clotting and bleeding processes throughout the body. DIC is almost always triggered by a major procedure or illness, such as cancer, severe injury, or most commonly, sepsis.
This is thought to be as a result of intense systemic inflammation leading to the release of pro-clotting factors into the bloodstream. A widespread activation of the clotting process leads to the formation of multiple small blood clots throughout the body's blood vessels, preventing blood flow to your cells and tissues, possibly resulting in tissue death.
As the clotting process progresses, it consumes the body's clotting factors and platelets, which are necessary for proper blood clotting. Once your body runs out of clothing factors and platelets, you shift into the second part of DIC, a state of uncontrolled bleeding.
Diagnosis
DIC typically begins with more mild symptoms before developing into the later stages of the condition.
- Fever
- Trouble catching your breath
- Low blood pressure
- Unprovoked/prolonged bleeding
- Pain/swelling in arms or legs
- Sudden confusion
This will then progress into overactive clotting and then bleeding which is typically how the condition is caught.
Diagnosis of DIC is typically made based on a physical exam and blood tests.
Treatment
DIC is a medical emergency and can be life-threatening. It is essential to seek immediate medical attention if you have any of the risk factors for DIC and begin to bleed excessively or without provocation. The earlier the condition is diagnosed and managed, the better the prognosis.
The typical treatment strategies include blood transfusions and/or anti-clotting medications (blood thinners). On top of the management of DIC itself, it is also essential to manage the underlying condition that led to this condition in the first place.
References
- Albagoush SA, Koya S, Chakraborty RK, et al. Factor V Leiden Mutation. [Updated 2023 Jan 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534802/
- Blood clotting disorders: Types, signs and treatment. Cleveland Clinic. (n.d.). Retrieved April 22, 2023, from https://my.clevelandclinic.org/health/diseases/16788-blood-clotting-disorders-hypercoagulable-states
- U.S. National Library of Medicine. (n.d.). Factor v Leiden thrombophilia: Medlineplus Genetics. MedlinePlus. Retrieved April 22, 2023, from https://medlineplus.gov
- U.S. Department of Health and Human Services. (n.d.). Blood Clotting Disorders: Types. National Heart Lung and Blood Institute. Retrieved April 22, 2023, from https://www.nhlbi.nih.gov
- Factor v leiden: Symptoms, causes & treatment. Cleveland Clinic. (n.d.). Retrieved April 22, 2023, from https://my.clevelandclinic.org
- Esmon, C T. “The normal role of Activated Protein C in maintaining homeostasis and its relevance to critical illness.” Critical care (London, England) vol. 5,2 (2001): S7-12. doi:10.1186/cc1333
- Prothrombin Gene Mutation: Symptoms, causes & treatment. Cleveland Clinic. (n.d.). Retrieved April 23, 2023, from https://my.clevelandclinic.org
- Jadaon, Mehrez M. “Epidemiology of Prothrombin G20210A Mutation in the Mediterranean Region.” Mediterranean journal of hematology and infectious diseases vol. 3,1 (2011): e2011054. doi:10.4084/MJHID.2011.054
- Bustamante JG, Goyal A, Singhal M. Antiphospholipid Syndrome. [Updated 2023 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430980/
- Antiphospholipid syndrome. (n.d.). Retrieved April 30, 2023, from https://rheumatology.org
- Overview: Antiphospholipid Syndrome. (n.d.). NHS choices. Retrieved April 30, 2023, from https://www.nhs.uk
- U.S. Department of Health and Human Services. (n.d.). Antiphospholipid syndrome (APS). National Heart Lung and Blood Institute. Retrieved April 30, 2023, from https://www.nhlbi.nih.gov
- Stello RA, Nehring SM. Disseminated Intravascular Coagulation. [Updated 2023 Jan 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441834/
- Disseminated intravascular coagulation (DIC): What is it, risk factors, symptoms & treatment. Cleveland Clinic. (n.d.). Retrieved April 30, 2023, from https://my.clevelandclinic.org
- U.S. Department of Health and Human Services. (n.d.). Disseminated intravascular coagulation (DIC). National Heart Lung and Blood Institute. Retrieved April 30, 2023, from https://www.nhlbi.nih.gov