What Is a Diabetic Eye Exam?
Why Does Diabetes Cause Eye Issues?
Diabetes can cause a variety of eye problems because of high blood sugar levels on the blood vessels and tissues in the eyes. When blood sugar levels are consistently high, it can damage the small blood vessels in the eyes. This damage can cause the blood vessels to:
- Become Leaky: High blood sugar can weaken the walls of the blood vessels, causing them to leak fluid or blood into the surrounding tissues. In the eyes, this leads to conditions like diabetic macular edema (DME), where fluid accumulates in the macula, the part of the retina responsible for sharp, central vision.
- Become Blocked: Damage to the blood vessels can cause them to become blocked or closed off, which deprives the retina of essential nutrients and oxygen. This can lead to the growth of new, abnormal blood vessels (neovascularization), which are prone to bleeding and can cause severe vision problems.
Diabetic Retinopathy
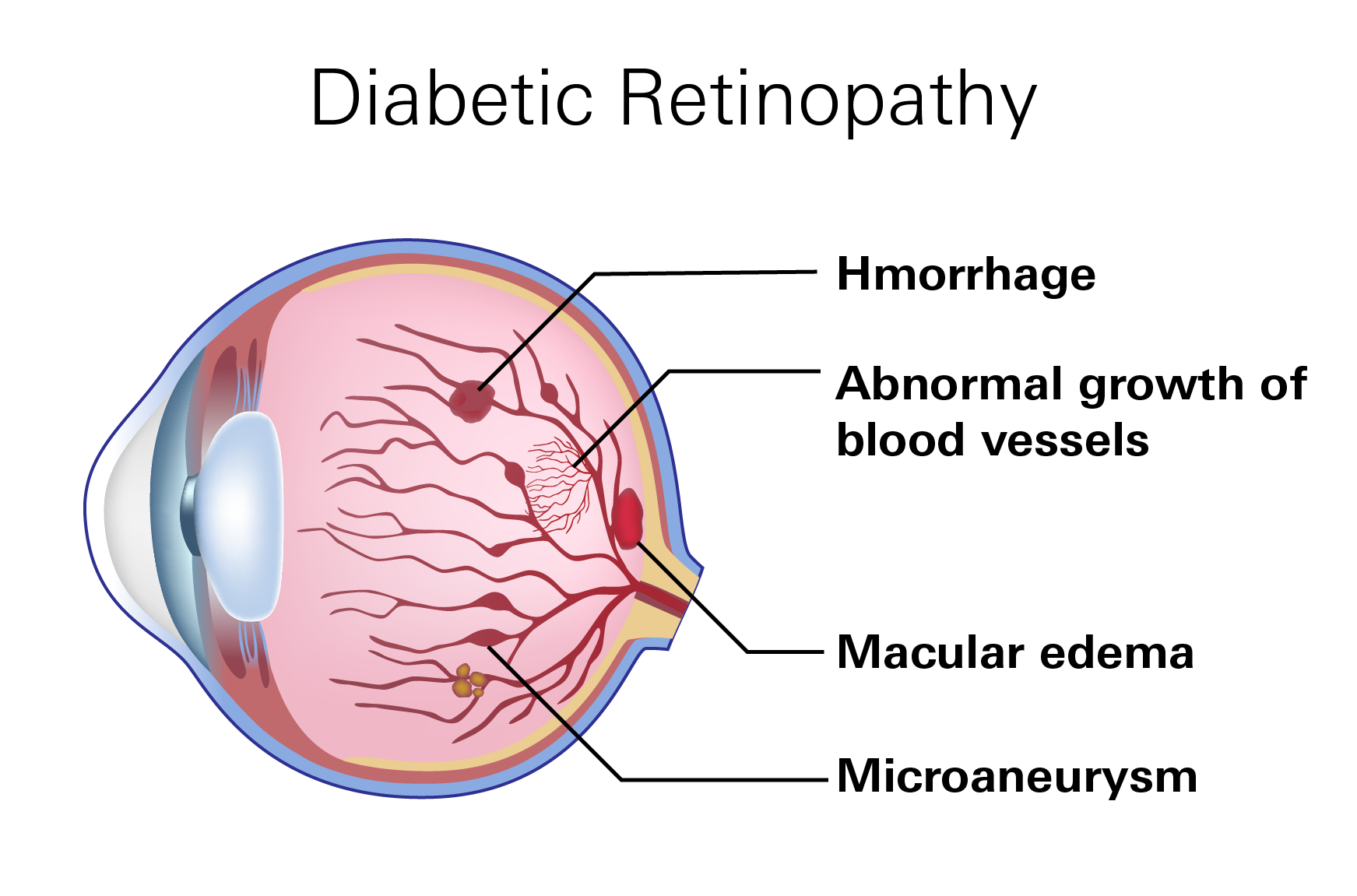
Diabetic retinopathy is a specific condition that results from damage to the blood vessels in the retina caused by prolonged high blood sugar levels. It progresses through stages from mild to severe, with increasing damage and potential vision loss as the condition advances. Key factors include:
- Microaneurysms: Small bulges in the blood vessels of the retina that may leak fluid.
- Retinal Hemorrhages: Bleeding from damaged blood vessels.
- Neovascularization: Growth of new, fragile blood vessels that can bleed and cause scar tissue to form.
In the early phases of diabetic retinopathy, vision changes and symptoms are not evident. The condition remains asymptomatic and can only be identified through an eye exam. This is why regular diabetic eye exams are crucial for early detection and management, helping to prevent or slow the progression of diabetic retinopathy.
Diabetic Macular Edema (DME)
DME is a complication of diabetic retinopathy where fluid leaks into the macula, causing it to swell. The macula is the part of the retina responsible for sharp, central vision, so swelling in this area can lead to distorted or blurred vision.
Symptoms of DME include:
- Blurry or wavy vision
- Difficulty reading
- Changes in color perception
Cataracts
People with diabetes are more likely to develop cataracts, a condition where the lens of the eye becomes cloudy. High blood sugar levels can cause changes in the lens proteins and its structure, leading to cloudiness and impaired vision.
Symptoms of cataracts include:
- Blurred or cloudy vision
- Sensitivity to glare, especially from lights at night
- Difficulty seeing well in low-light conditions
- Fading or yellowing of colors
Glaucoma
Diabetes increases the risk of developing glaucoma, a group of eye conditions that damage the optic nerve, often due to increased pressure inside the eye. High blood sugar levels can contribute to changes in the eye that increase this pressure, such as the formation of new blood vessels that block normal fluid drainage from the eye.
Symptoms of Glaucome include:
- Blurred or hazy vision
- Eye pain
- Gradual loss of peripheral vision: Glaucoma often affects peripheral vision first, leading to a gradual narrowing of the visual field.
- Halos around lights: Seeing halos around lights, particularly in low-light conditions, can be a symptom of increased intraocular pressure, a characteristic feature of glaucoma.
- Headaches: Elevated intraocular pressure can sometimes cause headaches.
Diabetic Eye Exam
Regular diabetic eye exams are crucial for maintaining eye health in individuals with diabetes. Even if your general doctor conducts routine eye checks, it is essential to undergo a comprehensive eye exam every 1 to 2 years with an ophthalmologist or optometrist. These specialized eye care professionals have the expertise and equipment necessary to detect subtle changes in the eye that may indicate the onset of diabetic eye diseases.
Key Components of a Diabetic Eye Exam
A diabetic eye exam includes several key tests that provide a thorough assessment of your eye health. While the specific procedures may vary depending on individual needs, the common components of a diabetic eye exam typically include the following:
Dilated Eye Exam
The dilated eye exam is a standard procedure where eye drops are used to dilate (widen) your pupils. This dilation allows the doctor to get a better view of the back of the eye, including the retina and the optic nerve. By examining these structures in detail, the doctor can detect signs of diabetic retinopathy, glaucoma, and other eye conditions that may not be visible with an undilated eye.
During this exam, the doctor looks for abnormalities such as microaneurysms (small bulges in blood vessels), hemorrhages, and signs of neovascularization (growth of new, abnormal blood vessels). These findings can indicate the presence and severity of diabetic retinopathy.
Visual Acuity Test
The visual acuity test measures how well you can see at various distances. Using a Snellen chart, which displays letters of varying sizes, the doctor determines the smallest letters or symbols you can read. This test helps assess the clarity and sharpness of your vision, providing a baseline for detecting changes over time.
Visual acuity tests are essential for identifying vision problems that may be caused by diabetic retinopathy, cataracts, or other conditions. Any significant changes in visual acuity can prompt further investigation and intervention.
Tonometry
Tonometry is a test that measures the pressure inside your eye, known as intraocular pressure (IOP). Elevated IOP is a major risk factor for glaucoma, a group of eye conditions that can lead to optic nerve damage and vision loss. People with diabetes are at an increased risk of developing glaucoma, making this test particularly important.
Several methods can be used to measure IOP, including non-contact tonometry (commonly known as the "air puff" test) and applanation tonometry, which involves direct contact with the eye. Both methods provide valuable information about eye pressure and help in the early detection of glaucoma.
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is an advanced imaging test that provides detailed cross-sectional images of the retina. This non-invasive test uses light waves to create high-resolution images, allowing the doctor to see the individual layers of the retina.
OCT is particularly useful for detecting diabetic retinopathy and diabetic macular edema (DME), a condition where fluid accumulates in the macula, the central part of the retina responsible for sharp, central vision. OCT can reveal retinal thickening, fluid accumulation, and other abnormalities that may not be visible during a standard eye exam.
Fluorescein Angiography
In some cases, the doctor may recommend fluorescein angiography, a procedure where a fluorescent dye is injected into your bloodstream. As the dye circulates through the blood vessels in the retina, photographs are taken to highlight any abnormalities. This test is especially useful for identifying leaking blood vessels, areas of non-perfusion (where blood flow is blocked), and abnormal blood vessel growth.
Fluorescein angiography provides detailed information about the blood flow in the retina and can help guide treatment decisions for diabetic retinopathy and other vascular conditions.
Why Regular Eye Exams Matter
Regular and comprehensive eye exams are essential for individuals with diabetes to monitor their eye health and detect any diabetes-related complications early. Early detection is critical because many diabetic eye diseases do not cause symptoms until significant damage has occurred. By the time symptoms like blurred vision, floaters, or vision loss become noticeable, the condition may already be advanced.
Early detection of diabetic eye diseases allows for timely intervention and treatment. For example, in the early stages of diabetic retinopathy, lifestyle changes and improved blood sugar control can help prevent further progression. In more advanced cases, treatments such as laser therapy, injections, or surgery can be effective in preserving vision.
Preventing vision loss is the primary goal of diabetic eye care. By detecting and managing eye conditions early, individuals with diabetes can maintain their vision and quality of life. Regular eye exams play a crucial role in achieving this goal.