Five Most Common Arrhythmias
What is an Arrhythmia?
An “arrhythmia” refers to any condition in which the heart rate or rhythm is not typical, including rhythms that are too fast, too slow, or irregular.
In typical adults, the heart beats at a rate of 60–100 beats per minute (bpm). Heart rhythm is a result of specific coordination of electrical signals throughout the heart. Sometimes there are problems within the system, and the rhythm loses its regularity.
How a Normal Heartbeat Works
In a very basic sense, the heart has 4 chambers: two on “top” (the atria) and two on the “bottom” (the ventricles). The atria and ventricles both have a left and right chamber.
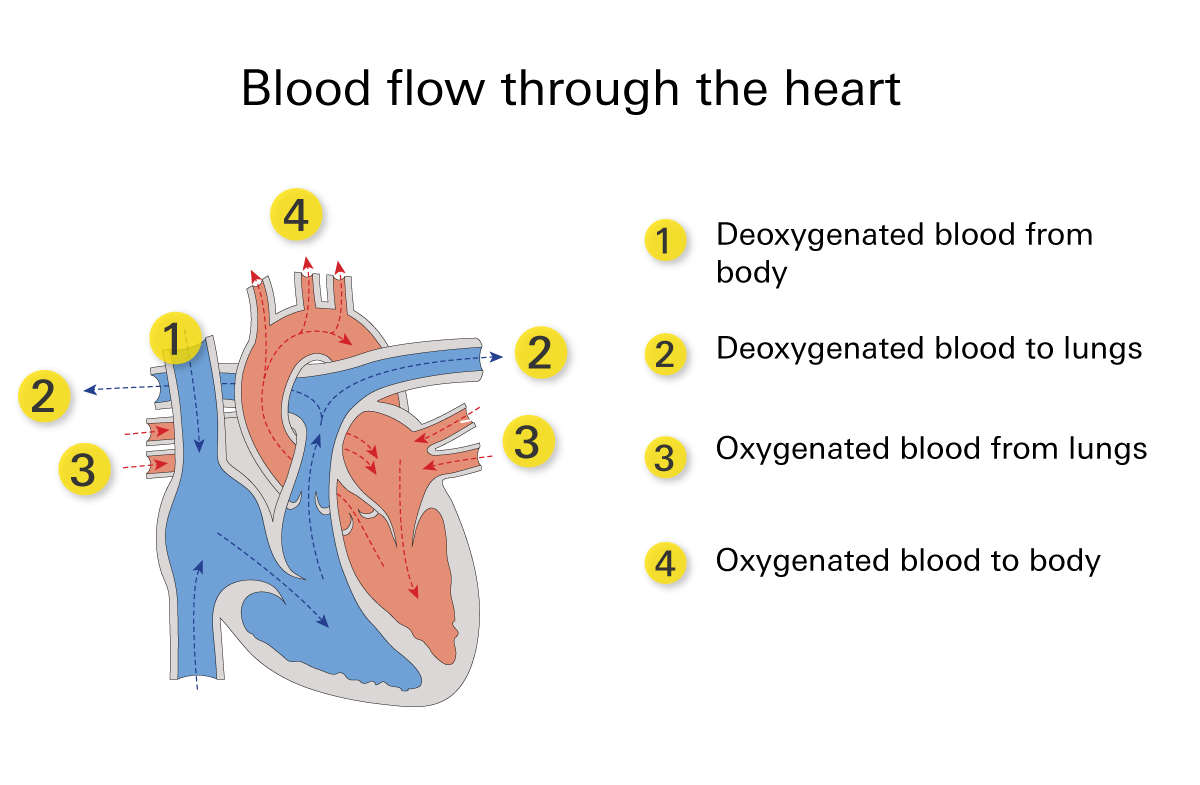
- Blood enters from the body, with low oxygen levels and full of waste, into the right atrium, which is then pumped into the right ventricle.
- From the right ventricle, the blood is pumped into the lungs. This is where the blood gets rid of its waste and gains more oxygen.
- The blood then enters the left atrium and is pushed into the left ventricle.
- From the left ventricle, the blood is squeezed into the body to provide our cells and tissues with oxygen.
To coordinate this activity, electricity makes its way through the heart.
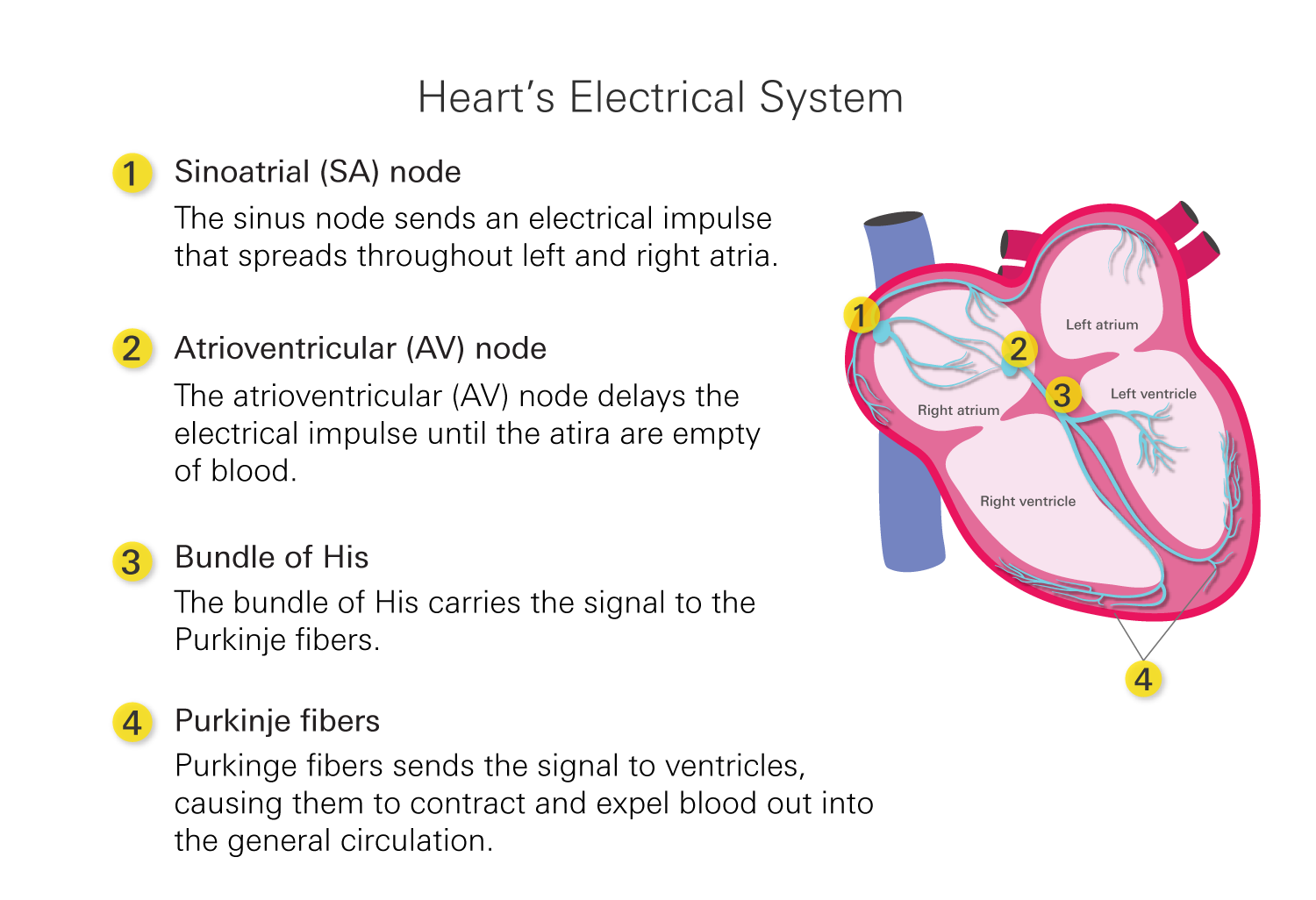
- The “SA node”, located in the right atrium, starts the beat by sending a signal through the heart for the atria to squeeze at the same time.
- This signal then makes its way to the down the heart to the AV node (also located in the right atrium). The AV node briefly delays the electrical impulse, allowing the atria to finish contracting and the ventricles to fill completely with blood.
- Once the ventricles are filled, the electrical signal rapidly travels down the bundle of His and reaches the Purkinje fibers.
- The Purkinje fibers distribute the electrical signal simultaneously throughout the ventricles, causing them to contract forcefully.
Since this system is so intricate and important, any interference can result in a change to the rhythm/rate of the heartbeat.
Types of Arrythmias
There are several types of arrhythmias, and they can be categorized based on their origin and the speed of heartbeats.
Bradycardia
Bradycardia (Brad-e-car-dee-uh) is a heart rate that is too slow. This is typically defined as an adult heart rate slower than 60bpm. This is dangerous because a heart rate that is too slow can result in an impairment in circulating oxygen-rich blood around your body. Often, this does not cause symptoms, but if the rate gets particularly slow (typically less than 40bpm) it can make you feel dizzy, tired, weak, and short of breath.
Causes
There are a number of possible causes of bradycardia, including;
- Problems with the SA nod
When the SA node stops conducting a regular heart rate, the AV node will typically take over. This results in a slowed heart rate of 40-60 bpm.
- Consequences of a heart related condition or event, such as a heart attack
Damage to the heart’s tissues can result in the slowed heart rate of bradycardia.
- Medications
Certain medications, particularly those that treat heart disease and high blood pressure, can often result in a slowed heart rate.
Treatment
There are three main methods of treatment for bradycardia, including:
- Removing anything that may be causing bradycardia
This is the first step when there is something preventable causing the bradycardia, such as a medication. Removing the medication and switching it for one that does not cause the slowed heart rate is often effective in speeding up the rate back to normal.
- Surgery
When the bradycardia is caused by something physically wrong with the heart, sometimes a surgery is able to remove or change the problem, restoring the regular rate.
- Pacemaker placement
When the other options are not available, a pacemaker is another effective solution to bradycardia. A pacemaker is a device that is surgically placed below your collarbone, with wires extending into your heart. A pacemaker is able to provide signals to your heart to beat on the occasion that your own heart’s conduction system misses a regular beat. This way it can make sure your heart does not beat at a rate below 60bpm.
Tachycardia
Tachycardia (tak-ee-car-dee-uh) is abnormal heart rate that is too fast. It is typically considered tachycardia when the heart rate is over 100bpm. Sometimes tachycardia is not harmful, such as with an increased heartrate during exercise or stressful situations.
If this is to occur at rest it can become dangerous, as a heart that beats too fast may not properly pump blood throughout the body. This may cause light-headedness, shortness of breath, and make you feel a racing sensation in your chest. There are many different types of tachycardia, some more dangerous than others. This includes sinus, ventricular, and supraventricular tachycardia.
Causes
The specific risk factors differ slightly depending on the specific form of tachycardia. In general, the factors that put you in more risk include:
- Heavily drinking alcohol, smoking, and/or using illicit street drugs (amphetamines, cocaine)
- Young age (children)
- Elderly individuals
- Those with certain heart conditions
- Use of certain prescription medications (levothyroxine, certain antidepressants)
Treatment
Ideally, prevention of tachycardia through risk factor modification is the best method to ensure normal rate when possible. Some risk factors are not modifiable, such as age. However, altering or discontinuing use of substances or prescription medications that increase your risk is often the first step in risk reduction.
When this is not an option, other alternatives for treatment of tachycardia include:
- Cardioversion
Cardioversion is a medication or electrical treatment given to individuals who have an abnormal rate or rhythm. It sends a kind of shock to the heart to cause a reset. Not everyone is a candidate for cardioversion, though it is often an effective method of restoring normal rate during tachycardia.
- Medications
There are certain medications that decrease heart rate and are often prescribed for other conditions such as high blood pressure. This includes beta-blockers, calcium channel blockers, and digoxin.
- Surgery
Depending on the cause of this arrhythmia, there are sometimes surgical interventions that can be used to fix this issue and restore normal rate.
- Pacemaker Placement
A pacemaker is a device that is surgically placed below your collarbone, with wires extending into your heart. A pacemaker is able to provide signals to your heart to beat on the occasion that your own heart’s conduction system misses a regular beat. This way it can make sure your heart does not exceed 100bpm.
Atrial fibrillation
Atrial fibrillation or “A fib” is the most common type of tachycardia. This abnormal rhythm occurs when the atria receive chaotic irregular signals resulting in an irregularly irregular beat. This rhythm can occur for short periods of time or can last indefinitely if left untreated.
A fib can lead to sensations of:
- Light-headedness
- Fluttering in your chest
- Fatigue
- Shortness of breath
As a result of these quick and chaotic contractions, blood gets left over in the atria and can even stay stagnant long enough to form clots. This leads to the greatest dangers of uncontrolled A fib, the increased risk of a stroke.
Causes
A fib can occur in anyone, and the cause is often unknown. However, there are some factors that may put you at increased risk. These include:
- Advanced age
- Uncontrolled high blood pressure
- Heart failure
- Hyperthyroidism
- Previous heart-related events, such as a heart attack
Treatment
There are a number of treatment strategies available for the treatment of A fib. Often a mix of strategies are used as the condition progresses.
- Medications
Rate control (bisoprolol, diltiazem, digoxin)—These medications work to decrease the heart rate to below 100bpm.
Rhythm control (amiodarone, lidocaine)—These medications work to restore normal regular rhythm.
Blood thinners (warfarin, apixaban)—These medications decrease the clotting of the blood to decrease the risk of stroke. - Cardioversion
Cardioversion is a medication or electrical treatment given to individuals who have an abnormal rhythm. It sends a kind of shock to the heart to reset its rhythm. Not everyone is a candidate for cardioversion, though it is often an effective method of restoring normal rhythm during A fib.
- Surgery
Depending on the cause of this arrhythmia, there are sometimes surgical interventions that can be used to fix this issue and restore normal rate.
- Pacemaker Placement
A pacemaker is a device that is surgically placed below your collarbone, with wires extending into your heart. A pacemaker is able to provide signals to your heart to beat on the occasion that your own heart’s conduction system misses a regular beat. This way it can make sure your heart does not exceed 100bpm.
Ventricular fibrillation
Ventricular fibrillation, or “V fib” is another type of tachycardia. It is an irregular rhythm resulting from uncoordinated electrical signalling through the ventricles. This prevents the filling and squeezing required for the heart to pump blood to the body. This is a very dangerous arrhythmia and can be fatal is not caught and treated quickly.
Causes
V fib is most frequently caused by a defect to the heart following an event such as a heart attack, or due to trauma to the heart such as heart surgery or a serious injury.
Treatment
V fib is a medical emergency and requires immediate intervention. Someone who is experiencing V fib will likely fall to the ground, unconscious, due to insufficient blood flow to the brain. They will require cardiopulmonary resuscitation (CPR) and, ideally, shocks to the heart with a defibrillator. A defibrillator works to send a shock to the heart, causing it to restart its normal rhythm.
After acute management of the condition, longer-term prevention is also often required. This would most likely include medication and/or the placement of an implantable cardiac defibrillator (ICD). These devices work by monitoring the heart’s rhythm and, if they pick up on any abnormalities, sending a shock to the heart to restore normal rhythm before any adverse events occur.
- Medications
Rate control (bisoprolol, diltiazem, digoxin)—These medications work to decrease the heart rate to below 100bpm.
Rhythm control (amiodarone, lidocaine)—These medications work to restore normal regular rhythm.
Blood thinners (warfarin, apixaban)—These medications decrease the clotting of the blood to decrease the risk of stroke. - Cardioversion
Cardioversion is a medication or electrical treatment given to individuals who have an abnormal rhythm. It sends a kind of shock to the heart to reset its rhythm. Not everyone is a candidate for cardioversion, though it is often an effective method of restoring normal rhythm during A fib.
- Surgery
Depending on the cause of this arrhythmia, there are sometimes surgical interventions that can be used to fix this issue and restore normal rate.
- Pacemaker Placement
A pacemaker is a device that is surgically placed below your collarbone, with wires extending into your heart. A pacemaker is able to provide signals to your heart to beat on the occasion that your own heart’s conduction system misses a regular beat. This way it can make sure your heart does not exceed 100bpm.
Long QT Syndrome
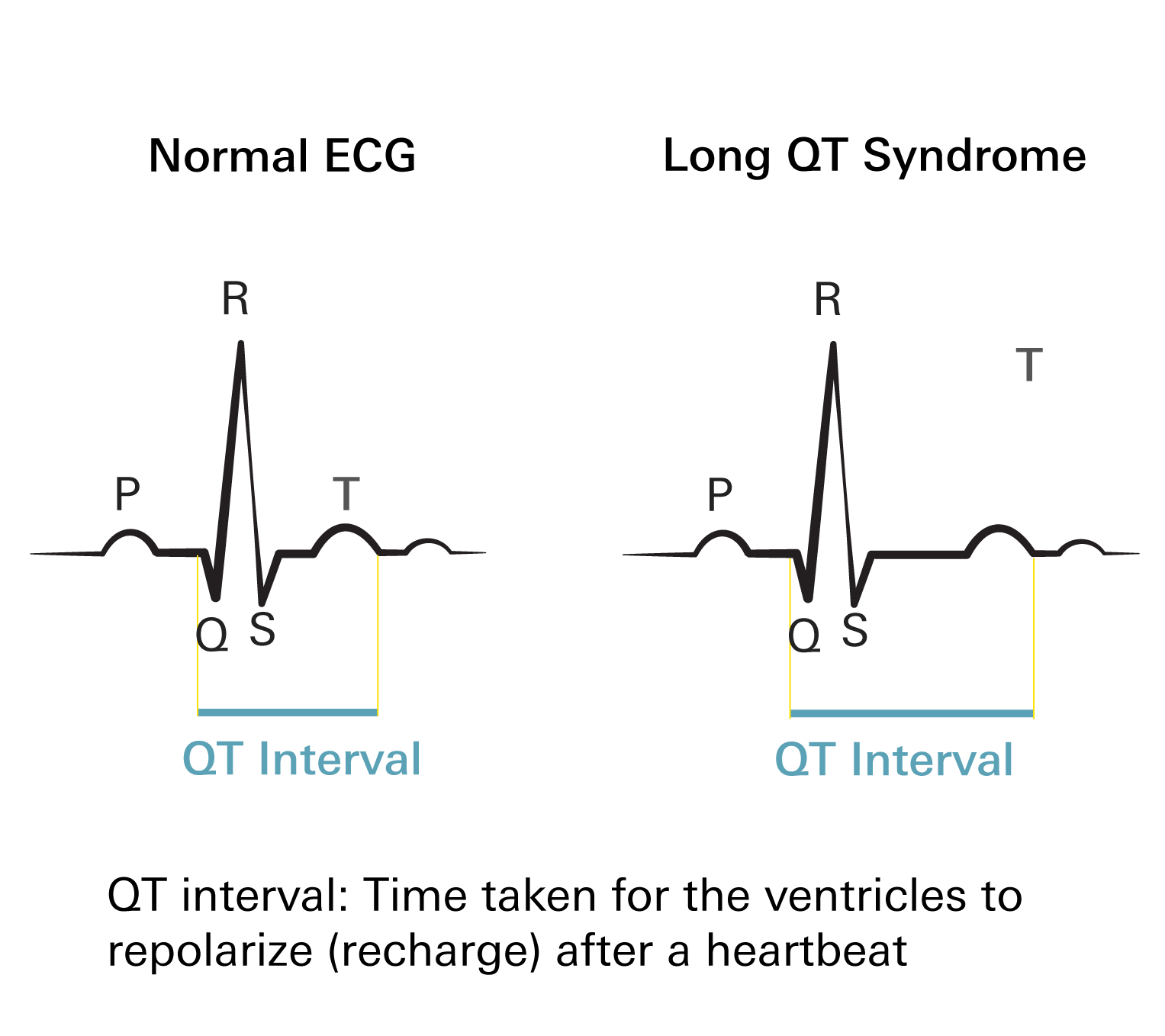
The heartbeat is often divided into sections labelled P, Q, R, S, and T.
The PR interval is the electrical activity that goes through the atria, while the Q-T interval involved the ventricular action. There is very specific timing for each of these sections, though sometimes this timing can be off.
When the Q-T interval is too long, this is termed “long QT”. This condition often does not cause any symptoms, though when it does these include light-headedness, weakness, blurred vision, and even fainting.
The main danger of long QT syndrome is that, if uncontrolled, it can sometimes turn into another condition called “Torsade de pointes” — a ventricular arrhythmia in which every beat looks different. This can then sometimes lead into V fib, which is life-threatening.
Causes
Often there is no known cause of long-QT syndrome. However, there are a number of factors that may increase your risk, including:
- Medications
Many medications prolong the QT segment of the heartbeat. This includes fluoroquinolone antibiotics (moxifloxacin, levofloxacin), antiarrhythmics (sotalol, quinidine), and many others.
- Certain acquired medical conditions
Certain conditions, such as hypothermia, a stroke, low calcium, and low potassium can lead to elongation of the QT interval.
- Genetic conditions of the heart
Sometimes people are born with genetic conditions that cause long QT. This includes both Romano-Ward Syndrome and Jervell and Lange-Nielsen Syndrome.
Treatment
If there is a clear cause of the long QT syndrome, the first step is to remove the causative factor. This could include warming someone up who is hypothermic or switching the antibiotic if using a fluoroquinolone.
If this is not a possibility, or in addition to removing the causative factor, there are also other options for controlling long-QT. This includes:
- Medications
There are a number of medications that revert the heart back to normal rhythm, including beta-blockers.
- Placement of an implantable cardiac defibrillator
o Implantable cardiac defibrillators (ICDs) work by monitoring the heart’s rhythm and, if they pick up on any abnormalities, send a shock to the heart to restore normal rhythm before any adverse events occur.
References
- Mayo Foundation for Medical Education and Research. (2022, May 7). Bradycardia. Mayo Clinic. Retrieved April 8, 2023, from https://www.mayoclinic.org
- Bradycardia: Slow heart rate. www.heart.org. (2023, April 5). Retrieved April 8, 2023, from https://www.heart.org
- WebMD. (n.d.). 6 medications that can causes changes to heart rate or rhythm. WebMD. Retrieved April 8, 2023, from https://www.webmd.com
- Tachycardia: Symptoms, causes & treatment. Cleveland Clinic. (n.d.). Retrieved April 8, 2023, from https://my.clevelandclinic.org
- WebMD. (n.d.). Tachycardia: Symptoms, causes, diagnosis, treatment. WebMD. Retrieved April 8, 2023, from https://www.webmd.com
- Tachycardia: Symptoms, causes & treatment. Cleveland Clinic. (n.d.). Retrieved April 8, 2023, from https://my.clevelandclinic.org
- Atrial fibrillation (AFIB): Causes, symptoms and treatment. Cleveland Clinic. (n.d.). Retrieved April 9, 2023, from https://my.clevelandclinic.org
- What is atrial fibrillation? - american heart association. (n.d.). Retrieved April 9, 2023, from https://www.heart.org
- Masoudi, Frederick A et al. “Longitudinal study of implantable cardioverter-defibrillators: methods and clinical characteristics of patients receiving implantable cardioverter-defibrillators for primary prevention in contemporary practice.” Circulation. Cardiovascular quality and outcomes vol. 5,6 (2012): e78-85. doi:10.1161/CIRCOUTCOMES.112.965368
- Ventricular fibrillation. www.heart.org. (2022, November 15). Retrieved April 9, 2023, from https://www.heart.org
- Long QT syndrome. Heart and Stroke Foundation of Canada. (n.d.). Retrieved April 9, 2023, from https://www.heartandstroke.ca