Top OTC Products for Managing Eczema
Eczema is a common inflammatory skin condition characterized by red, itchy, and inflamed skin. It can affect individuals of all ages, though it is most frequently seen in children.
Types of Eczema
-
 Atopic Dermatitis: The most common form of eczema, often beginning in childhood. Symptoms include red, itchy rashes that can become thickened and scaly, frequently affecting the face, hands, feet, and the inside of elbows and knees.
Atopic Dermatitis: The most common form of eczema, often beginning in childhood. Symptoms include red, itchy rashes that can become thickened and scaly, frequently affecting the face, hands, feet, and the inside of elbows and knees. -
 Contact Dermatitis: Caused by skin contact with allergens or irritants. Symptoms include red, itchy, and burning rashes in the area of contact.
Contact Dermatitis: Caused by skin contact with allergens or irritants. Symptoms include red, itchy, and burning rashes in the area of contact. -
 Dyshidrotic Eczema: Affects the hands and feet, causing small blisters. Symptoms include small, deep-seated blisters that are intensely itchy, followed by cracking, scaling, or peeling of the skin.
Dyshidrotic Eczema: Affects the hands and feet, causing small blisters. Symptoms include small, deep-seated blisters that are intensely itchy, followed by cracking, scaling, or peeling of the skin. -
 Nummular Eczema (Discoid Eczema/Nummular Dermatitis): Appears as patches on the skin that may ooze or become very sensitive and dry. Symptoms include round, itchy, and sometimes oozing patches of skin, often on the arms, legs, hands, or torso.
Nummular Eczema (Discoid Eczema/Nummular Dermatitis): Appears as patches on the skin that may ooze or become very sensitive and dry. Symptoms include round, itchy, and sometimes oozing patches of skin, often on the arms, legs, hands, or torso. -
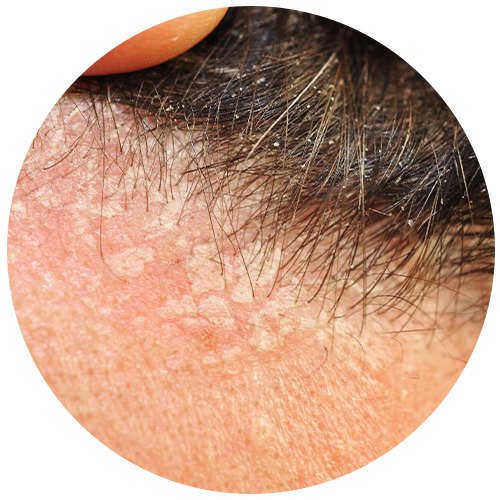 Seborrheic Dermatitis: Often occurs on the scalp. Symptoms include scaly patches, redness, and stubborn dandruff, commonly on the scalp and oily areas of the face.
Seborrheic Dermatitis: Often occurs on the scalp. Symptoms include scaly patches, redness, and stubborn dandruff, commonly on the scalp and oily areas of the face. -
 Stasis Dermatitis: Also referred to as gravitational dermatitis, venous eczema, or venous stasis dermatitis. Occurs in the lower legs due to poor circulation. Symptoms include swollen, itchy skin, often with varicose veins, and can lead to open sores or ulcers.
Stasis Dermatitis: Also referred to as gravitational dermatitis, venous eczema, or venous stasis dermatitis. Occurs in the lower legs due to poor circulation. Symptoms include swollen, itchy skin, often with varicose veins, and can lead to open sores or ulcers.
Top over-the-Counter (OTC) Products For Eczema
OTC treatments provide accessible and immediate relief from itching, redness, and inflammation. While they can be effective, their success often depends on the severity of your condition. For mild to moderate cases, OTC medications can significantly reduce symptoms and improve quality of life. However, in more severe cases, prescription medications or other treatments may be necessary.
The National Eczema Association recommends several OTC products that contain:
Emollients
Emollients are substances that soften and moisturize the skin. Emollients form a protective barrier on the skin to retain moisture and prevent dryness. They are a key ingredient in moisturizers designed for eczema care. This barrier provides relief from dryness, flakiness, and irritation.
Common emollients include petroleum jelly, mineral oil, lanolin, and glycerin.
Types of Emollients
There are two main types of emollients, each serving a unique function in skincare:
- Occlusives: Occlusives form a thick, greasy coating on the skin that does not dissolve in water. They do not add moisture to the skin but help it retain the moisture it already has. By creating a barrier, occlusives prevent water from evaporating from the skin’s surface. Common examples of occlusives include:
- Petroleum jelly
- Mineral oil
- Lanolin
- Liquid paraffin
- Humectants: Humectants attract and bind water to the skin, increasing its moisture content. These ingredients are less thick and greasy compared to occlusives and can wash off more easily in water. Humectants are particularly effective in drawing moisture from the environment into the skin, making it feel hydrated and supple. Common examples of humectants include:
- Glycerin
- Hyaluronic acid
- Propylene glycol
- Urea
Many moisturizing skincare products contain a combination of both occlusives and humectants to provide comprehensive hydration and protection for the skin. Look for thick, fragrance-free moisturizers. Products containing ceramides are particularly effective as they help restore your skin barrier. Ointments containing lanolin are more occlusive and can be very effective in locking in moisture.
Recommended products include:
- Vaseline Pure Petroleum Jelly
- CeraVe Healing Ointment
- CeraVe Moisturizing Lotion
- Gold Bond Eczema Relief Cream
- Gold Bond Ultimate Eczema Relief
Antihistamines and Eczema
Atopic dermatitis is part of the atopic triad, which includes eczema, allergies, and asthma. Due to this connection, healthcare providers may recommend antihistamines to help reduce itching and inflammation triggered by allergies. However, antihistamines are generally not considered a first-line treatment for eczema itself.
Some studies have found limited evidence supporting the effectiveness of antihistamines in treating eczema directly. The quality of this evidence is not strong, and more research is needed to fully understand the role of antihistamines in managing eczema symptoms. Nonetheless, antihistamines may still be beneficial in reducing itching, especially in cases where eczema is aggravated by concurrent allergies.
Common Oral Antihistamines:
- Diphenhydramine (Benadryl)
- Fexofenadine (Allegra)
For managing common symptoms such as burning, pain, or inflammation, over-the-counter pain relievers can be helpful. The following are commonly used:
- Acetaminophen (Tylenol)
- Ibuprofen (Motrin, Advil)
Topical Steroids for Eczema
Topical steroids can be effective in reducing inflammation and promoting healing during mild to moderate eczema flare-ups. However, using stronger steroids or applying them for extended periods can lead to permanent side effects, such as skin thinning (atrophy) and discoloration. To minimize risks, it’s important to use the lowest effective dose for the shortest duration necessary, typically applying them 1 to 4 times per day.
- Hydrocortisone 1%: This is a common and mild steroid cream available OTC, suitable for short-term use in mild cases of eczema.
- Cortizone-10 Intensive Healing Eczema Care: This product is specifically formulated to manage eczema symptoms, combining hydrocortisone with moisturizers to enhance skin healing.
Tips to Help Reduce Eczema Flare-Ups
Eczema flare-ups can be disruptive, but there are effective strategies to minimize their frequency and severity. Here are a few key practices:
- Identify and Avoid Triggers: Pinpoint and avoid your personal triggers, such as specific foods, detergents, soaps, dust mites, pollen, or even wool clothing.
- Maintain a Healthy Skin Barrier: Regularly apply fragrance-free moisturizers, even during clear periods. This helps keep your skin's natural barrier strong, preventing flare-ups
- Choose Comfortable Clothing: Opt for soft, breathable, loose-fitting clothes to minimize irritation.
- Gentle Skincare Routine: Use mild, fragrance-free soaps and shampoos to avoid further irritation. Steer clear of products containing alcohol, dyes, or strong perfumes.
- Stress Management: Reduce stress, as it can aggravate eczema. Relaxation techniques like yoga or meditation can be beneficial.
- Stay Cool: Overheating can trigger flare-ups, so keep your environment cool and avoid sweating excessively.
- Warm Baths: Opt for short, lukewarm baths instead of long, hot showers. Hot water can strip your skin of natural oils. Always moisturize immediately after bathing.
When to Speak with a Doctor About Eczema
You should speak with your doctor about eczema and the use of OTC medications if your symptoms persist or worsen despite treatment, if you experience severe flare-ups, or if you notice signs of infection like increased redness, warmth, or pus. It is also important to consult with a pharmacist or doctor if you are unsure which OTC medication to use or if frequent use of OTC products isn’t providing long-term relief.
Commonly Asked Questions About Eczema
Click the question below to expand on the answer
Can over-the-counter products help treat eczema?
Yes. Over-the-counter (OTC) products can help manage mild eczema by moisturizing the skin and calming inflammation. Fragrance-free creams with ceramides, urea, or glycerin help repair the skin barrier, while 1% hydrocortisone creams can reduce redness and itching during flare-ups.
For more severe or persistent symptoms, prescription-strength treatments may be needed. But for mild eczema, consistent use of OTC moisturizers and gentle cleansers can make a big difference.
Which over-the-counter products are best for mild eczema?
For mild eczema, common OTC options include fragrance-free moisturizers with ceramides, urea or glycerin; mild hydrocortisone 1% creams for occasional flare-ups; and gentle non-soap cleansers to reduce dryness and irritation.
When should I see a doctor instead of relying on OTC treatments?
If your eczema covers a large area, is extremely painful or bleeding, is getting worse despite consistent OTC use, or you have signs of infection — it’s time to talk to your healthcare provider. Often prescription treatments are needed for moderate-to-severe eczema or skin in sensitive areas and our provider can help you make an informed decision on how best to treat it.
How often should moisturizers be used for eczema?
Moisturizers are a foundational part of eczema care and should ideally be applied at least once daily — more often if your skin feels very dry. Using them consistently helps reduce flare-ups and improves skin barrier health.
Can daily lifestyle changes help with my eczema?
Yes. Avoiding hot showers, using lukewarm water, choosing fragrance-free skincare, avoiding harsh detergents, and managing stress are all helpful. These steps reduce skin irritation, preserve the barrier function, and make your treatment efforts more effective.
What triggers eczema flare-ups?
Eczema flare-ups can be triggered by a variety of factors that irritate or dry out the skin. Common triggers include cold, dry weather, hot showers, and harsh soaps or detergents that strip away natural oils.
Other triggers include stress, allergies (such as dust, pollen, or pet dander), sweating, and certain fabrics like wool or synthetic fibers. Even scratching can worsen irritation and create a cycle of itch and inflammation.
Identifying and avoiding your personal triggers—while keeping skin well moisturized—can help reduce flare-ups and make eczema much easier to manage.
Can eczema be cured?
Eczema isn’t currently curable, but it can be well controlled with the right care. Many people experience long periods of clear skin when they consistently manage their symptoms and avoid known triggers.
Treatment focuses on restoring the skin barrier, relieving itching, and reducing inflammation. Daily moisturizers, gentle cleansers, and occasional use of medicated creams during flare-ups can make a big difference.
In some cases, eczema may even improve or disappear over time—especially for children—but it can return if the skin becomes dry or irritated again.
Can eczema go away on its own?
In some cases, yes — especially in children, eczema can fade or disappear completely as the skin barrier strengthens with age. However, for many people, eczema is a chronic condition that comes and goes over time.
Even if symptoms improve, the underlying sensitivity of the skin often remains. Flare-ups may return when the skin becomes dry, irritated, or exposed to triggers such as stress or allergens.
While eczema may not permanently go away, consistent skincare and early treatment of flare-ups can help you keep symptoms under control and enjoy long periods of clear skin.
Do kids with eczema always grow up to have eczema as an adult?
Not always. Many children with eczema see their symptoms improve or even disappear as they get older. In fact, about half of children with eczema experience significant improvement by their teenage years.
However, some continue to have sensitive or dry skin as adults, and flare-ups may return later in life—especially during times of stress, illness, or skin irritation. People with a family history of allergies or asthma are more likely to have long-term eczema.
Even if eczema improves with age, maintaining good skin hydration and avoiding triggers can help prevent it from coming back.
References:
- National Eczema Association. (n.d.). Eczema: Causes, Symptoms, and Treatments. Retrieved from https://nationaleczema.org/eczema/
- Coulson, I. H., & Graham-Brown, R. A. C. (2019). Antihistamines for eczema. Cochrane Database of Systematic Reviews, 2019(2), Art. No.: CD012167. https://doi.org/ 10.1002/14651858.CD012167.pub2