Rheumatoid Arthritis: An Autoimmune Disease
Every year, 71 out of every 100,000 individuals are diagnosed with rheumatoid arthritis
What is Rheumatoid Arthritis (RA)?
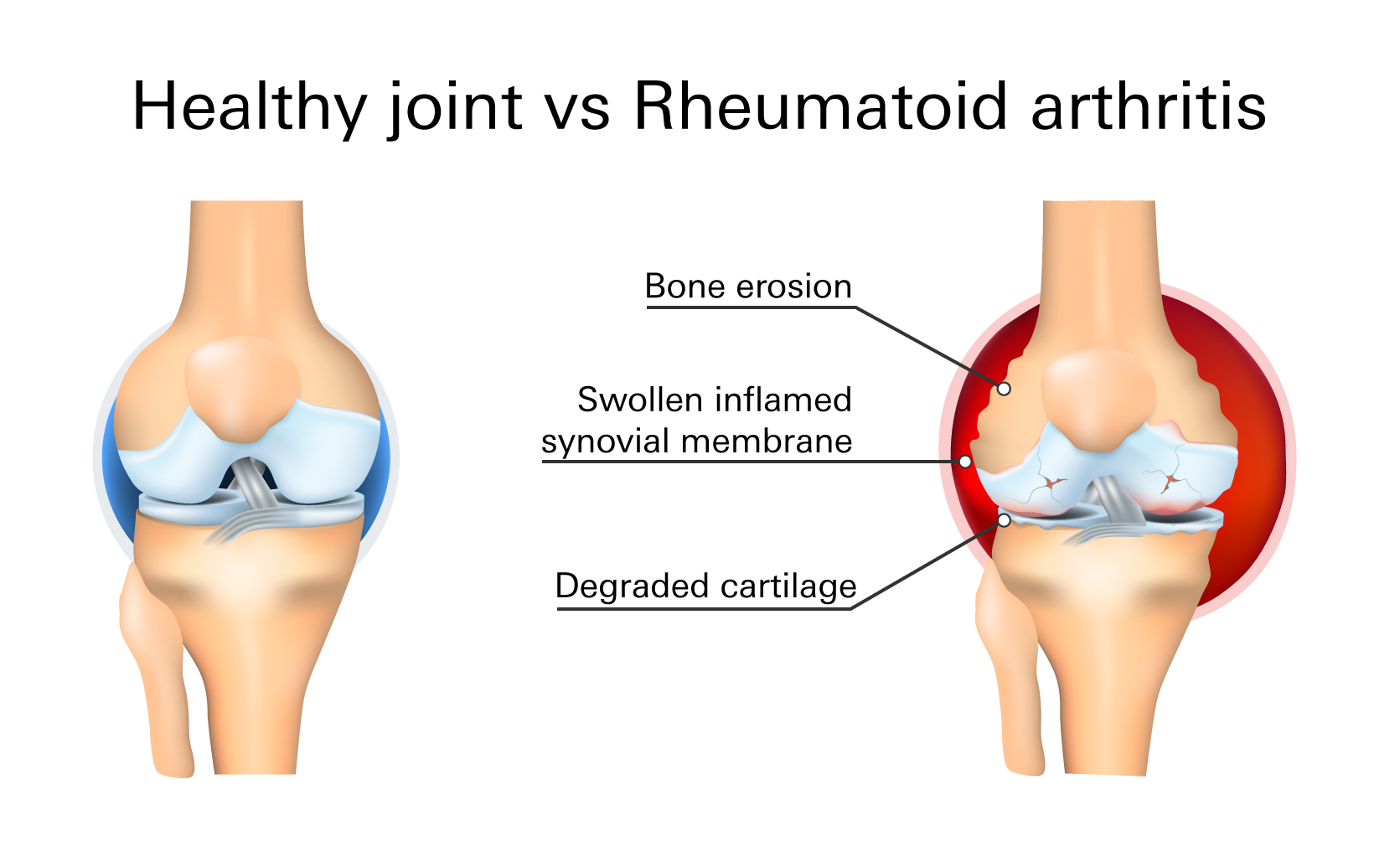
Rheumatoid arthritis (RA) is a chronic/long-term, progressive autoimmune disorder (when your body's tissues are attacked by your immune system), that primarily affects your joints. Other organs in your body, such as your kidneys, lungs, heart, blood vessels, and eyes can be affected as well.
Symptoms
Rheumatoid arthritis results in warm, tender, swollen, and painful joints. This autoimmune disease generally presents in the smaller joints of your fingers, wrist, ankles, and feet first.
- joint swelling
- pain
- stiffness
- bone deformity
- weakness and/or fatigue
- loss of appetite
- difficulty moving
- edema (swelling)
- fever
- redness
Stiffness and pain are worse after rest which is why “morning stiffness” is a common complaint.
The intensity and recurrence of rheumatoid arthritis symptoms may vary. Times of relative remission, during which the swelling and discomfort subside or go away, alternate with periods of increased disease activity, or flares. Rheumatoid arthritis can cause joints to distort and move out of place over time.
Diagnosis
Diagnosis will depend on a combination of signs and symptoms.
- Blood tests: Blood tests examine for blood proteins (antibodies) and inflammation, both of which are correlated with RA. Rheumatoid factor (RF) and rheumatoid- citrullinated peptide antibody (ACPA) are measured in the lab tests.
- Physical exam: Your rheumatologist will check for bumps beneath your skin, joint soreness, swelling, warmth, and painful or limited movement.
- Imaging tests: The ends of your bones within a joint may deteriorate (erosions) because of rheumatoid arthritis. A scan using an MRI, ultrasound, or X-ray can screen for erosions.
Treatment
Even with the tremendous improvements in treatment options, severe RA can still result in physical impairments.
The main goals of RA treatment are to reduce pain, inflammation, and joint destruction. Most individuals are advised to take medications that can reduce or even stop joint degeneration.
Non-medical treatments for rheumatoid arthritis include rest/relaxation, physical therapy, occupational therapy, exercise, diet, and managing your weight.
Medical treatment
(Non-biologic) Disease-modifying anti-rheumatic drugs (DMARDs)—first-line drug treatment for RA
Patients with symptoms of RA should be started on a DMARD, regardless of the severity of the disease. DMARDs slow the disease process and help prevent further joint damage. The treatment goal is remission of the disease (or low disease activity).
Methotrexate
Brands: Trexall (oral tablet), Otrexup (subcutaneous needle), Rasuvo (subcutaneous needle), Xatmep (oral solution for children)
Preferred as initial therapy for most patients with RA.
Administration: 2.5 mg taken every 12 hours, 3 doses per week
Side effects: nausea, vomiting, diarrhea, stomatitis (inflamed and sore mouth), sensitivity to sunlight, joint pain, muscle pain.
Black box warning (the strictest warnings for prescriptions): Methotrexate may cause severe liver damage (alcohol use can increase the risk of liver toxicity), decrease bone marrow activity (myelosuppression), and should not be used to treat arthritis when pregnant since it may harm or kill the fetus.
Hydroxychloroquine (Plaquenil)
Administration: 400 mg daily (initially), then 300 mg daily (as a maintenance dose). Take it with food or milk.
Side effects: nausea, vomiting, diarrhea, abdominal pain, rash, headache, vision changes.
Sulfasalazine (Azulfidine)
500–1,000 mg initially, then 1,000 mg twice a day.
Take it food or a cup (8 oz.) of water to prevent crystalluria (crystals in your urine, indicating renal irritation.
Side effects: headache, rash, nausea, vomiting, diarrhea, folate deficiency, crystalluria, yellow-orange discoloration of your skin and/or urine.
Leflunomide (Arava)
Administration: 100 mg taken for 3 days, then 20 mg taken daily
Side effects: nausea, diarrhea, rash, headache, respiratory infections, chest pain/discomfort
Black box warning: Should not be used to treat arthritis when pregnant since it may harm or kill the unborn child, as well as severe liver damage.
Tofacitinib (Xeljanz, Xeljanz XR)
Administration: 5 mg twice a day. XR: 11 mg daily
Side effects: upper respiratory tract infection (URTI), urinary tract infection (UTI), diarrhea, headache, high blood pressure
Baricitinib (Olumiant)
Administration: 2 mg daily
After previous therapies have failed, patients with rheumatoid arthritis can use baricitinib to relieve pain, stiffness, and swelling.
Side effects: shortness of breath, nausea, vomiting, chest pain/pressure, weakness on one side of your body
Biologic DMARDs
For people who do not respond to non-biologic DMARD therapy or who have severe rheumatoid arthritis, further therapies are available. A biologic DMARD can be used in place of another DMARD or as a stand-alone therapy.
This drug class of medications is administered as subcutaneous (SC) injections (injected under your skin) and works by targeting immune system pathways. They frequently block a variety of inflammatory proteins, receptors, and cells.
Examples of biologic DMARDs:
- Etanercept (Enbrel): 50 mg SC weekly
- Adalimumab (Humira): 40 mg SC every other week
- Certolizumab pegol (Cimzia): 400 mg SC at weeks 0, 2, and 4, then 200 mg SC every other week
- Golimumab (Simponi): 50 mg monthly
Side effects: infections and injection site reactions, such as: rash, swelling, itching, and bruising, headache, nausea.
Speak With Your Doctor
If you experience ongoing joint pain and swelling, consult your doctor and send your prescription to Marley Drug. Save up to 95% compared to your local pharmacy by using Marley Drug.