What is Gastroparesis?
About of 100,000 people, approximately 10 men and 40 women have gastroparesis.
What is gastroparesis?
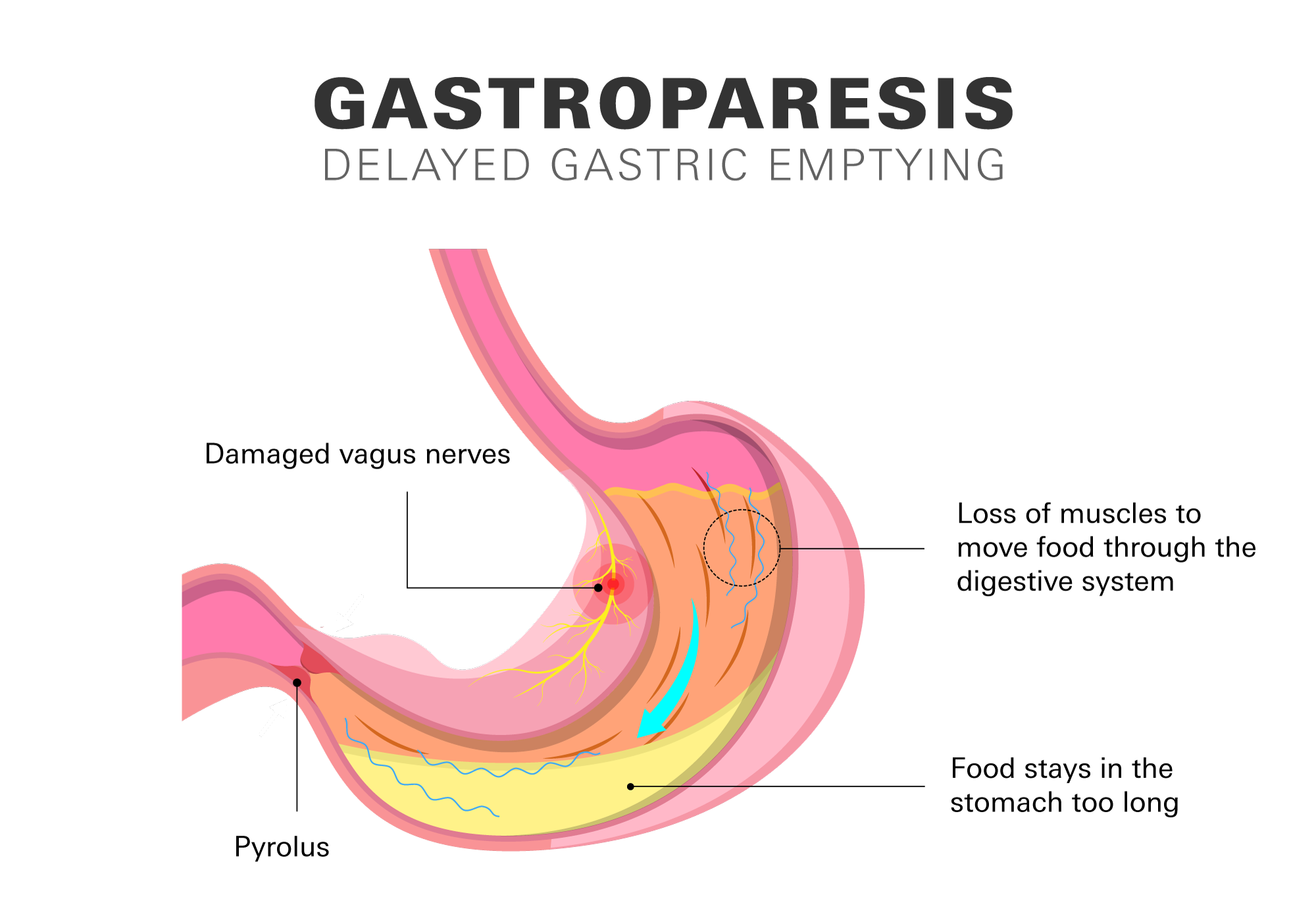
Gastroparesis is a medical condition characterized by delayed emptying of the stomach. The term "gastroparesis" is derived from the Latin words "gastro" meaning stomach and "paresis" meaning partial paralysis. In this condition, the muscles in the stomach fail to function properly, resulting in a slowdown or partial paralysis of the stomach's ability to empty its contents into the small intestine.
The normal functioning of your digestive system involves a complex process that includes nerve and muscle activity. As food enters your stomach, it’s broken down by your stomach acid and digestive enzymes, and then gradually passed into your small intestine for further digestion and absorption of nutrients.
With gastroparesis food stays in your stomach for a long time, resulting in painful symptoms. You can have instant and prolonged feelings of fullness after eating. You might feel queasy, vomit, or experience stomach pain. You can have acid reflux as a side effect along with feeling bloated or distended (stretched) in your stomach. Heartburn symptoms can occur when stomach acid backwashes into the esophagus.
Although gastroparesis is not a life-threatening condition, it is a debilitating illness that can significantly impact your quality of life. Management of gastroparesis typically involves a combination of lifestyle changes, medications, and in some cases, surgical intervention.
How common is gastroparesis?
Although the exact prevalence is unknown, gastroparesis is considered an uncommon condition. An estimated 1.5 million Americans, or 0.5% of the population, live with gastroparesis, according to estimates from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Despite the fact that gastroparesis can affect individuals of any age, it is typically diagnosed in adults between the ages of 40 and 60. It's important to note that women are more likely than men to have this condition.
Types of gastroparesis
Depending on what's causing it, medical professionals frequently divide gastroparesis into 3 main categories.
- Diabetic gastroparesis: gastroparesis that develops as a complication of diabetes. High blood sugar levels over time can damage the nerves that control stomach motility, leading to delayed gastric emptying. Diabetic gastroparesis is one of the most common causes of gastroparesis.
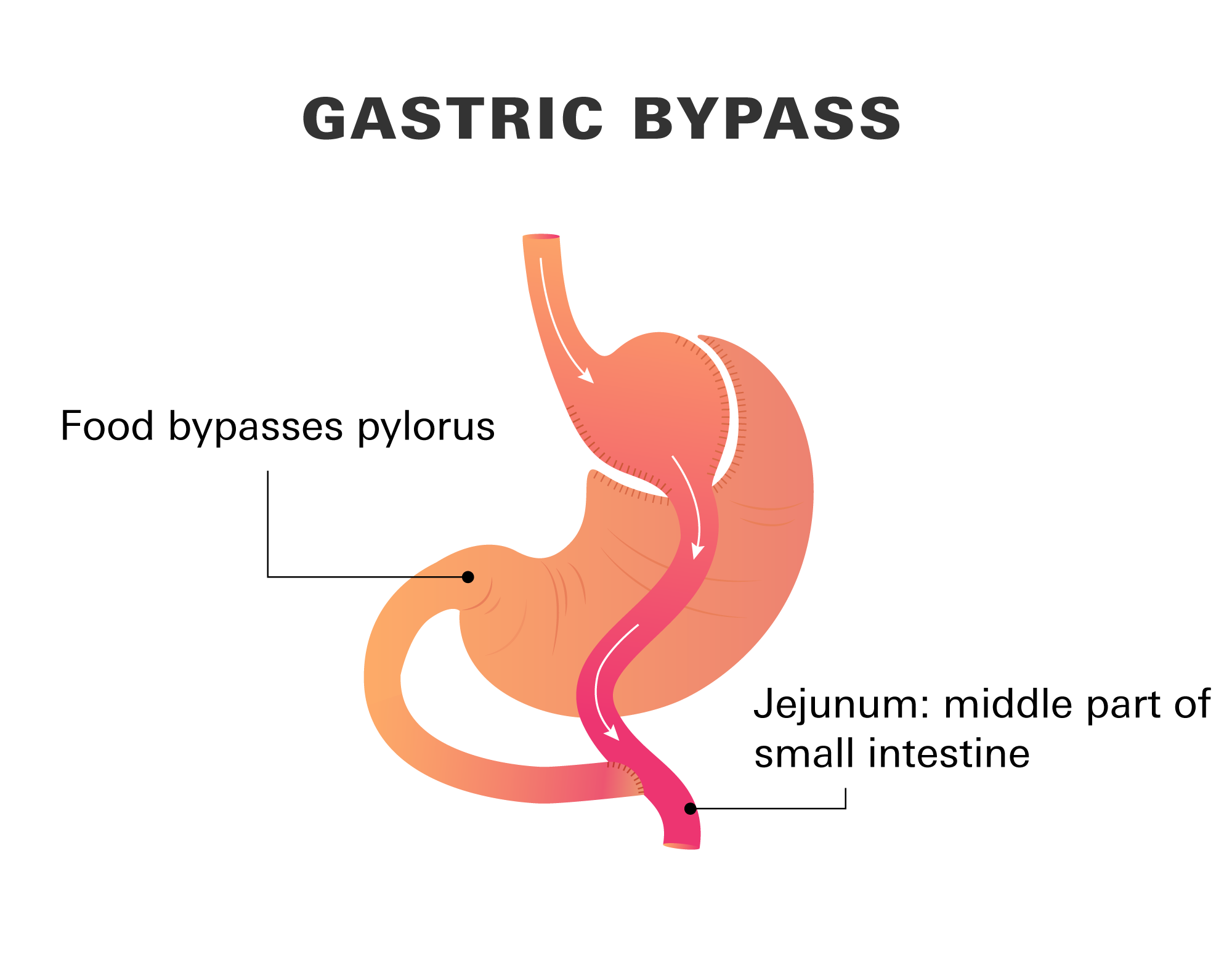
- Post-surgical gastroparesis: Some individuals may develop gastroparesis as a complication following certain surgical procedures involving the stomach or intestines. Examples include gastric bypass surgery or other abdominal surgeries.
- Idiopathic gastroparesis:It refers to gastroparesis for no known cause. In these cases, thorough investigations have been conducted, but no specific underlying cause has been identified.
Signs and symptoms of gastroparesis
- Nausea
- Vomiting
- Acid reflux
- Stomach bloating
- Fluctuations in blood sugar levels
- Heartburn
- Indigestion
- Decreased appetite
- Upper stomach pain
- Constipation
- A sensation of satiety after consuming a small meal
- Vomiting undigested food eaten a few hours earlier
- Decreased weight and/or malnutrition
Although symptoms of gastroparesis may vary between person to person, it’s important to keep in mind that some individuals with this condition may not have any signs or symptoms.
Are bowel movements affected by gastroparesis?
Your entire digestive system is slowed down by gastroparesis, which can cause a delay in bowel movements. It can also send large, undigested food fragments to your intestines, where they can be more challenging to pass through. Although gastroparesis doesn't directly alter how your intestines move, several of the conditions that contribute to it can.
Causes and risk factors
Gastroparesis can be caused by a range of factors that disrupt the normal motility of the stomach. The main factor is damage to the nerves that control your stomach muscles.
- Diabetes
High blood sugar levels can damage the nerves that control the muscles of your stomach, leading to delayed gastric emptying. - Neurological disorders
Certain neurological conditions such as Parkinson's disease, multiple sclerosis, and amyloidosis can affect the nerves that control your stomach. - Viral infections
Some viral infections, including norovirus or rotavirus, can damage the nerves that control the muscles of your stomach, leading to gastroparesis. - Surgery
Certain types of surgery, such as gastric bypass surgery or surgeries that involve the vagus nerve, can damage the nerves or muscles that control your stomach. - Autoimmune disorders
In rare cases, gastroparesis may be caused by an autoimmune disorder that affects the nerves of your stomach. - Medications
Some medications can cause gastroparesis as a side effect, including opioids, some antidepressants, and medications used to treat high blood pressure, including calcium channel blockers (CCBs), as well as marijuana. - Idiopathic gastroparesis
In some cases, no underlying cause for gastroparesis can be identified. As mentioned, this is known as idiopathic gastroparesis.
However, the exact cause of gastroparesis can be difficult to determine, and a thorough medical evaluation is often necessary to identify the underlying cause of the condition.
Risk factors
The following variables may increase your likelihood of developing gastroparesis:
- Abdominal or esophageal surgery
- Diabetes
- Infection, typically caused by a virus
- Hypothyroidism
- Parkinson's disease or multiple sclerosis
How is gastroparesis diagnosed?
There are several ways to diagnose gastroparesis. Your doctor may use one or more of the following tests to diagnose gastroparesis and determine the underlying cause of the condition.
- Gastric emptying study: This test, also called a gastric emptying scan, shows how fast food leaves your stomach after consuming a small meal.
- Breath test: This test, also called a gastric motility breath test (GEBT), involves consuming a small meal and then measuring the amount of carbon dioxide in your breath. Elevated levels of carbon dioxide may indicate gastroparesis.
- Electrogastrography (EGG): This test measures the electrical activity of the stomach muscles to evaluate their function.
- Upper gastrointestinal (GI) endoscopys: This test uses a thin, flexible tube with a camera on the end to examine the inside of your esophagus, stomach, and small intestine (duodenum).
- Blood tests: These tests can be used to rule out other conditions that may be causing symptoms similar to gastroparesis.
What are treatment options for gastroparesis?
The treatment options for gastroparesis depend on the severity of the condition, the underlying cause, and the individual's overall health status.
Medications
Prokinetic agents and antiemetics are the main drug classes used to treat gastroparesis. Prokinetic agents help stimulate the contractions of the stomach muscles to move food through the system. Antiemetic medications help relieve nausea and vomiting associated with gastroparesis.
- Metoclopramide (brand: Reglan): The only FDA has approved prokinetic agent tog to treat gastroparesis. It induces abdominal muscle contractions and may also be used to manage nausea. It does, however, have a black-box label warning since it may result in adverse effects such as tremors and muscle twitching.
- Domperidone: Domperidone is a prokinetic and a dopamine receptor antagonist. Domperidone appears to be as effective as metoclopramide for the treatment of gastroparesis symptoms but tends to have less adverse effects that are connected to the nerve and brain.
- Promethasine: Promethazine is a type of antihistamine drug that also functions as an antiemetic. Promethazine is used for naasea and vomitting, but unlike prokinetics, it has little effect on stomach emptying.
- Ondansetron (brand: Zofran): Another antiemetic drug that can be used to treat gastroparesis-related nausea is ondansetron. It functions by preventing your body's natural chemical messenger, serotonin, from doing its job.
- Erythromycin: A macrolide antibiotic called erythromycin also has prokinetic properties. Erythromycin works by accelerating the rate at which food leaves your stomach, reducing gastroparesis symptoms. However, after 4 weeks of therapy, this medication's effects may decrease. It’s best utilized for short periods of time.
Surgery
In severe cases, surgery may be necessary to remove the portion of your stomach that is not working properly.
- Pyloroplasty
Pyloroplasty is a surgical procedure that involves widening the opening between the stomach and the small intestine called the pylorus. Pylorus is the muscle valve that allows food to exit from your stomach. By enlarging the pylorus valve, the stomach can empty more quickly. - Gastric bypass
The lower part of your stomach may need to be totally bypassed, either because it is no longer functional or because this surgery has a higher chance of success. A type is gastic bypass is gastrojejunostomy (GAS-troh-JEH-joo-NOS-toh-mee) where part of your stomach is removed, and a new passageway from your stomach to the middle part (jejunum) of the small intestine is made, bypassing the pylorus.Gastric bypass is frequently recommended as a weight-loss procedure for those with type 2 diabetes.
- Gastric electrical stimulation (GES)
This surgical procedure involves the placement of a device called a gastric stimulator or neurostimulator. The device is implanted in the abdomen and delivers electrical impulses to the stomach muscles, helping to improve gastric motility and reduce symptoms. GES is typically considered for individuals with refractory gastroparesis (gastroparesis that doesn't respond to other treatments). It can be done using minimally invasive laparoscopic techniques.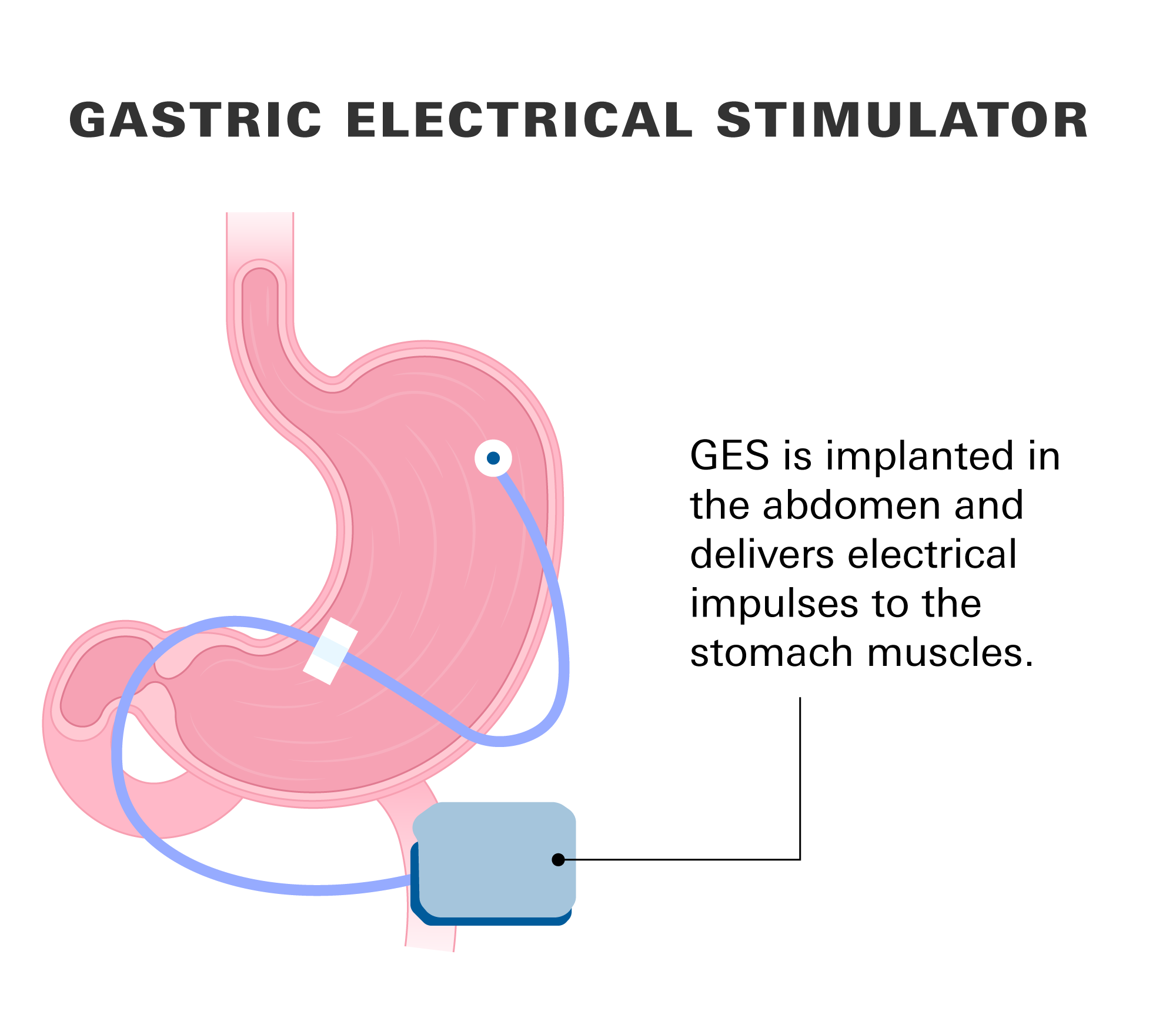
Dietary modifications
You may need to follow a low-fat and low-fiber diet that is easy to digest. Small, frequent meals may be recommended to help with stomach emptying.
Nutritional support
In some cases, nutritional support may be necessary, such as the use of enteral feeding or parenteral nutrition.
It is important to consult with a healthcare professional for an accurate diagnosis and individualized treatment plan.