- Athlete's foot is a common fungal infection of the feet, thriving in warm, damp environments like sweaty shoes and public showers.
- Symptoms typically include itchy, red, peeling, or cracked skin, often between the toes or on the soles.
- Most cases can be treated with over-the-counter antifungal creams, but severe or persistent infections may require prescription medication.
- Prevention involves keeping feet dry, wearing breathable footwear, and avoiding walking barefoot in communal damp areas.
Overview
Athlete’s foot is a common skin infection caused by fungi that live on the outer layer of the skin. It often starts as a red, itchy, or stinging rash between the toes or on the bottom of the foot.


These fungi thrive in warm, damp environments like sweaty shoes, boots, or thick socks. You can easily pick it up by walking barefoot on contaminated surfaces such as locker-room floors or communal showers.
Symptoms often include redness, itching, or peeling skin between the toes or on the arch of the foot. While called "athlete's foot," anyone can get it, not just athletes. If left untreated, the infection can spread to toenails or lead to bacterial infections.
How Common is It?
Epidemiology reviews estimate that about 10% of the U.S. population—roughly 1 in 10 Americans—will experience athlete’s foot in any given year. This means millions are affected annually. Health-care records reinforce this, showing that out of approximately 6 million annual visits for superficial fungal skin infections, tinea pedis (athlete’s foot) accounts for just over 12%, about 730,000 office visits each year.
Symptoms
Athlete’s foot can show up in different ways, but most cases share a few common signs:
- Itchy skin, especially when it’s warm or sweaty
- Red or scaly rash on the toes, soles, or sides of the foot
- Burning or stinging feeling, sometimes before a rash appears
- Cracked or peeling skin, which can bleed if deep
- Dry, rough patches, especially on the heel or arch
- Strong foot odor, worse than normal sweat
- Tingling or prickling before visible symptoms
- Thick, yellowish toenails if the fungus spreads under the nail
Types of Athlete’s Foot and How They Look
| Pattern | Toe-web (interdigital) |
|---|---|
| Typical Spot | Spaces between the fourth and fifth toes (may spread to others) |
| Skin Changes | Soft, soggy skin that whitens, peels, or splits into fine cracks |
| Observations | Persistent itch, mild burning after removing shoes, faint musty odor |
| Pattern | Moccasin (hyperkeratotic) |
|---|---|
| Typical Spot | Soles, heels, and sides of the foot |
| Skin Changes | Dry, flaky scales that thicken and form rough plaques; deep heel cracks possible |
| Observations | Achy step when fissures stretch; fine powder inside socks |
| Pattern | Vesicular (blistering) |
|---|---|
| Typical Spot | Arch or ball of the foot |
| Skin Changes | Small, clear blisters filled with fluid; burst blisters leave pinpoint raw spots |
| Observations | Tingling or “pins-and-needles” before blisters; mild swelling |
| Pattern | Ulcerative/mixed |
|---|---|
| Typical Spot | Starts between toes, can extend across the sole |
| Skin Changes | Shallow open sores or ragged ulcers that may ooze |
| Observations | Redness, warmth, yellow crust (signs of bacteria); painful walking |
Causes
Athlete’s foot is caused by a group of molds known as dermatophytes. The most common types are Trichophyton rubrum, T. interdigitale, and their close relatives. These fungi are hardy and can survive in many environments, but they especially thrive when skin is kept warm and damp, like inside sweaty shoes or boots.
How Infection Happens
- Entry Point: The fungus needs a small break in the skin to start an infection. This could be a tiny scratch from tight shoes, a small cut from nail clipping, or any minor abrasion.
- Feeding Ground: Once inside, the fungus feeds on keratin, a protein found in the outer layer of skin.
How It Spreads
- Direct Contact: Sharing a shower stall, touching bare feet on a yoga mat, or living with someone who already has athlete’s foot can transfer the infection.
- Contact with Contaminated Objects: Items like towels, socks, rental skates, pool deck tiles, and bathroom rugs can carry microscopic flakes of infected skin. Even one flake can start a new outbreak.
Feet are especially at risk because they often spend hours sealed inside shoes, where sweat accumulates and ventilation is poor. This creates the perfect environment for fungal spores to activate and multiply. If the infection isn’t treated and the conditions persist, the same fungi can spread from the skin into the toenails, causing a stubborn nail infection that is much harder to eliminate.
Who’s at Risk for Athlete’s Foot?
Certain habits, environments, and health conditions make it easier for the fungus that causes athlete’s foot to grow and spread. Here are the most common risk factors:
Moisture
- Sweaty feet, especially in people with hyperhidrosis (excessive sweating), create the perfect environment for fungus.
- Wearing damp socks or not giving shoes time to dry out increases the risk.
Tight or Non-Breathable Footwear
- Shoes that trap heat and moisture, like rubber boots or tight athletic shoes, encourage fungal growth.
- Footwear made from materials that don’t breathe well makes things worse.
Barefoot Contact with Shared Wet Surfaces
- Places like locker rooms, public showers, pool decks, and gym mats often carry fungal spores.
- Sandals or water shoes can help protect against exposure.
Skin Breaks or Friction
- Small cuts, blisters, or rubbing from tight shoes give the fungus an easy way into the skin.
Sharing Personal Items
- Using someone else’s towel, socks, shoes, or nail clippers can spread the infection.
Health Conditions
- People with diabetes, poor circulation, or weakened immune systems are more likely to get infected and heal more slowly.
- Long-term use of steroids or chemotherapy can also lower the skin’s defenses.
Hot, Humid Environments
- Living in tropical climates or working in hot, sweaty conditions (like construction) raises the risk.
Age and Gender
- Adult men are more likely to get athlete’s foot than women or children, possibly due to sweat levels and footwear choices.
Diagnosis
Most clinicians can spot athlete’s foot with a simple look at the skin. Peeling between the toes, fine white scale on the sole, or small fluid-filled blisters form a pattern that stands out.
If the rash is unclear, a doctor may scrape a bit of flaky skin, mix it with potassium hydroxide, and examine it under a microscope. The chemical clears normal cells and leaves branching fungal strands that settle the question. For stubborn or repeat infections, the sample can be grown in an incubator or tested to identify the exact species.
Treatment
Treating athlete’s foot means two things: killing the fungus and keeping your feet dry.
Mild cases often clear up with over-the-counter (OTC) antifungal creams or sprays. More serious or stubborn infections may need prescription medication.
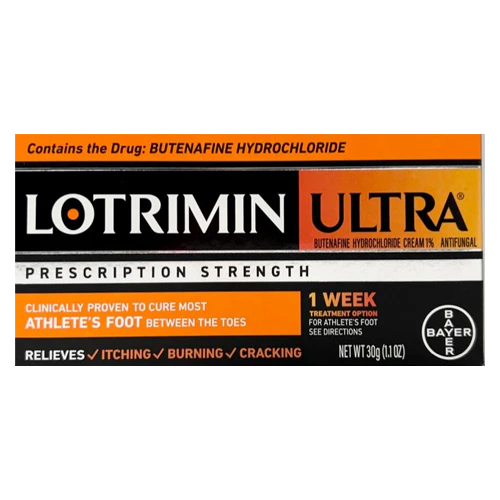
Over-the-Counter Antifungal Treatments
| Tolnaftate (Tinactin) |
|---|
|
| Clotrimazole (Lotrimin AF) |
|
| Terbinafine (Lamisil AT) |
|
| Miconazole |
|
Always read the package instructions, as directions can vary by brand.
Prescription Options
| Clotrimazole + Betamethasone (Lotrisone) |
|---|
|
Combines antifungal and corticosteroid to reduce inflammation and itch. Apply a thin layer twice daily for 2 weeks (max 45 grams/week); discontinue by week 4 even if some redness remains. |
| Econazole 1% (foam or cream) |
|
Apply once daily for 4 weeks. |
| Sulconazole (Exelderm) |
|
Thin applications twice daily for 4 weeks. |
| Ketoconazole |
|
Oral dose for adults typically starts at 200 mg daily, may increase to 400 mg. |
Home Remedies and Supportive Care
- Foot hygiene: Reduces moisture and fungal load.
- Sock and shoe rotation: Cuts down on humidity and allows drying.
- Vinegar soaks: Lowers skin pH, slowing fungal growth.
- Tea tree oil: Mild natural antifungal; may help with odor.
- Baking soda: Absorbs moisture and neutralizes odor.
It’s important to keep in mind that home methods can soothe and support, but should never replace proven antifungal medicines.
It’s recommended to receive medical guidance if your rash worsens, fails to improve after 2 weeks of diligent OTC use, or if you have diabetes, poor circulation, or a weakened immune system.
Prevention
A few everyday habits can make life hard for the fungus that causes athlete’s foot.
- Keep the skin bone-dry: After every shower, dab each foot until no moisture hides between the toes. If the towel misses a spot, a quick blast of cool air from a hair-dryer finishes the job.
- Change socks: Fresh, breathable socks each morning, and again whenever the first pair feels damp, pull sweat away from the skin. Give yesterday’s shoes a full day to air out before you step back into them.
- Pick shoes that breathe: Mesh athletic shoes or soft leather loafers let heat escape. When heavy boots are unavoidable, switch to lighter footwear as soon as the task is done.
Related Topics
Naftifine Cream for Athlete’s Foot and More
Naftifine cream is a prescription topical antifungal medication to treat skin infections such as athlete’s foot, ringworm, and jock itch. It stops the growth of fungi on the skin to clear the infection.
Read more