- Cervical cancer is caused by persistent HPV infection; develops slowly over 10–20+ years from precancerous changes.
- Often no early symptoms. That's why regular screening (Pap/HPV tests starting at age 21) is critical to catch and treat changes before cancer forms.
- Highly preventable. HPV vaccination and routine screening dramatically reduces risk.
- When detected early through Pap or HPV tests, the 5-year survival rate is over 90%.
Overview
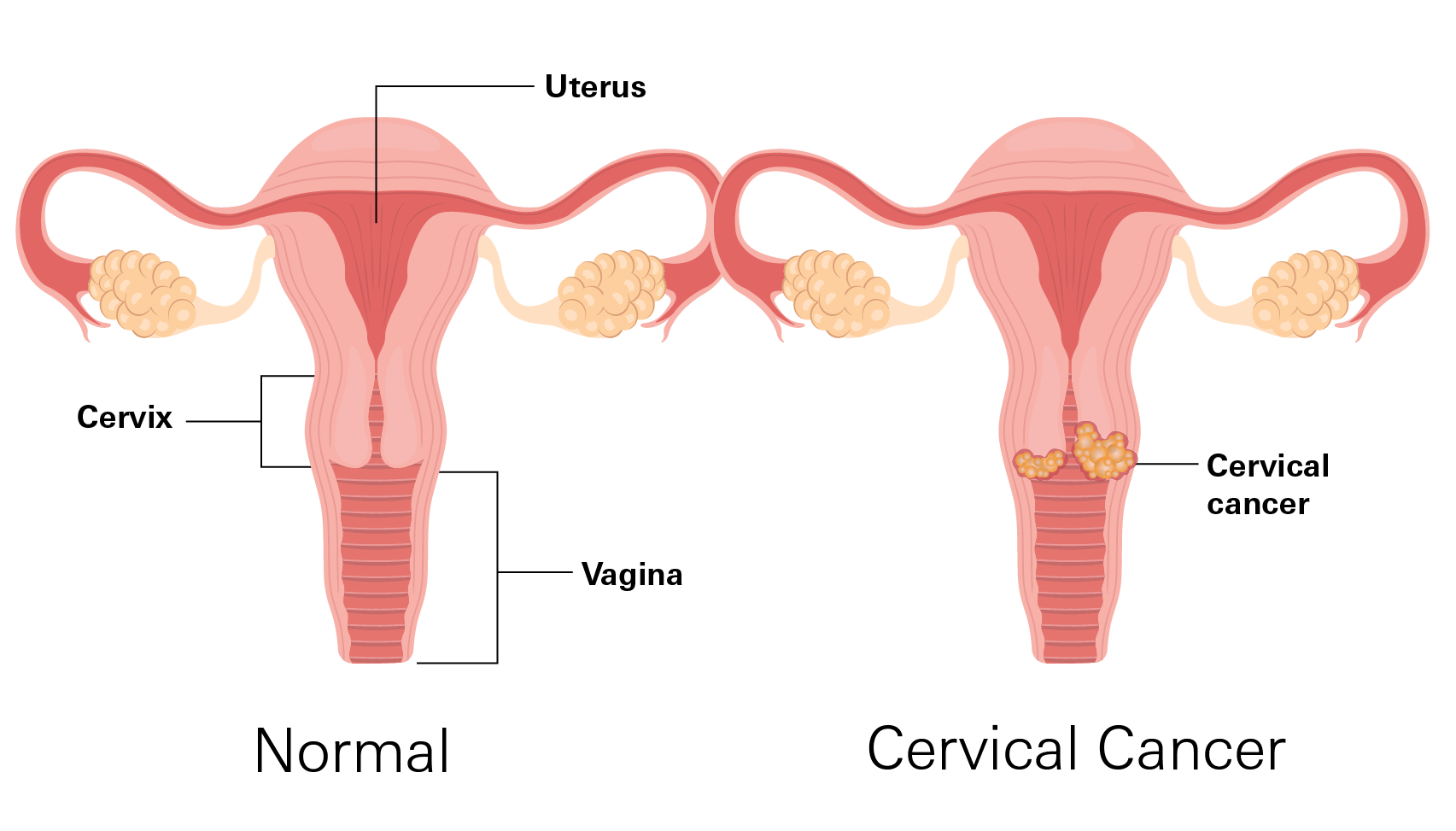
Cervical cancer starts in the cervix, the lower part of the uterus that connects to the vagina. Because of its location, abnormal cell changes can often be found early through routine screening like Pap tests or HPV tests.
Cancer develops when normal cells stop following their usual life cycle. Instead of growing and dying in an orderly way, abnormal cells continue to multiply. Over many years, these abnormal cells can become precancerous changes and, if untreated, may eventually develop into cervical cancer.
Most cervical cancers develop slowly. Many precancerous changes never turn into cancer, especially when found early through screening. When caught early, the five-year survival rate exceeds 90%.
How common is it?
Cervical cancer is a global health issue, but its impact varies dramatically depending on access to vaccination, screening, and treatment.
- Globally: It is the 4th most common cancer in women. In 2022, there were approximately 660,000 new cases and 350,000 deaths. Notably, 94% of these deaths occurred in low- and middle-income countries due to limited access to prevention and treatment.
- In the U.S.: Around 14,000 women are diagnosed annually. Thanks to widespread Pap testing, the mortality rate has dropped by nearly 75% over the last several decades.
- Age: Most diagnoses occur between ages 35 and 44, though more than 20% of cases are found in women over 65 (often after regular screening has stopped).
Symptoms
Cervical cancer often develops without early symptoms, which is why regular screenings matter.
As it progresses, symptoms can appear but might be mild or intermittent.
- Unusual vaginal bleeding: Between periods, after sex, or after menopause.
- Abnormal vaginal discharge: Watery, heavy, or blood-tinged, sometimes with a strong odor.
- Pelvic pain or pressure: Discomfort not linked to the menstrual cycle.
- Pain during sex: Often a sign of more advanced disease.
In advanced stages, symptoms may worsen:
- Ongoing pelvic or back pain
- Swelling in the legs
- Trouble urinating or having bowel movements
- Fatigue that doesn’t improve with rest
If you notice these, see a doctor promptly. Early action improves outcomes.
Types
Cervical cancers are classified by the type of cell where the cancer first started.
- Squamous cell carcinoma: The most common type (around 90% of cases). It forms in the flat cells on the surface of the cervix (exocervix). These changes are often detected through Pap tests.
- Adenocarcinoma: Begins in the gland cells lining the cervical canal (endocervix). These are higher inside the cervix, making early changes harder to detect.
- Adenosquamous carcinoma (mixed type): Contains features of both squamous and gland cells.
Stages
Staging describes how far the cancer has grown or spread. This helps guide treatment and gives a clearer picture of what to expect.
Stage 0 (precancer)
Abnormal cells are only on the surface layer of the cervix. They haven't grown deeper into the tissue yet. This isn't true cancer, but treating it now prevents cancer from developing.
Stage I: The cancer is only in the cervix
- Stage IA: Very small. Can only be seen under a microscope (not visible during a regular exam).
- Stage IB: Larger and visible. Subdivided by size:
Smaller tumors (up to about 4 cm, roughly the size of a walnut).
Larger tumors (bigger than 4 cm).
At this stage, the outlook is often very good with treatment.
Stage II: The cancer has grown beyond the cervix but not too far.
It may spread to the upper part of the vagina (the canal leading to the outside) or the tissue around the uterus (womb). It hasn't reached the pelvic walls (the sides of the pelvis) or the lower vagina yet.
Many cases at this stage can still be treated successfully.
Stage III: The cancer has spread farther within the pelvis.
It may reach the lower part of the vagina, the pelvic walls, nearby lymph nodes, or cause issues like blocking the tubes that carry urine from the kidneys to the bladder (leading to kidney swelling).
Treatment is still possible, often with a combination of approaches.
Stage IV (the most advanced)
The cancer has spread outside the pelvis to nearby organs (Stage IVA: bladder, rectum) or to distant parts of the body (Stage IVB: lungs, liver, bones).
Even at this stage, treatments can help manage symptoms and improve quality of life.
Note: Cervical cancer usually grows slowly, so catching it early (stage 0–I or II) makes a big difference. Survival rates are much higher.
Cuases
Main cause: Persistent HPV infection
Nearly all cervical cancers are caused by long‑term infection with high‑risk types of human papillomavirus (HPV). HPV is extremely common, spread through intimate skin‑to‑skin contact, and usually cleared by the immune system within 1–2 years.
Cancer risk rises when HPV remains in the cervix for many years, interfering with normal cell growth. For most women, progression from persistent HPV to cancer takes 15–20 years. It may happen faster in women with weakened immune systems.
Risk Factors
- Persistent HPV infection: The main cause.
- Weakened immune system: Women with HIV are 6x more likely to develop cervical cancer
- Not getting screened regularly: Abnormal cells go undetected.
- Smoking: Damages cervical cells and weakens local immune defenses
- Long-term use of hormonal contraceptives: Slightly increases risk
- Pregnancy-related factors: Having three or more full-term pregnancies, or a first pregnancy before age 20, may increase risk.
- Age: Most cases occur in mid-adulthood, reflecting the disease’s slow development.
Diagnosis
Cervical cancer often causes no symptoms in its early stages. Diagnosis usually begins with routine screening rather than waiting for physical signs.
Main screening tests:
- Pap test: Looks for abnormal cell changes on the cervix
- HPV test: Detects high-risk strains of HPV that can cause cervical cancer.
Screening Recommendations
- Ages 21–29: Pap test every 3 years if results are normal.
- Ages 30–65: One of the following approaches may be used
- HPV test alone every 5 years, or
- HPV test plus Pap test every 5 years, or
- Pap test alone every 3 years.
When screening may no longer be needed:
- Women over age 65 who have had several years of normal results and no history of serious cervical abnormalities may stop screening permanently.
- Those who have had a total hysterectomy (uterus and cervix removed) may stop screening unless surgery was done for cancer or serious precancer.
Screening remains important even for women who have been vaccinated for HPV or have had children, since vaccination does not protect against every cancer-causing HPV type.
Treatment
If cancer or precancer is found, treatment is personalized based on the stage of the disease, its location, and your future plans for pregnancy.
Surgery
Used mainly for early-stage cancer or precancer. The goal is to remove or destroy abnormal tissue while preserving healthy areas.
- Ablation: Destroys abnormal tissue without removing it, often with freezing (cryotherapy) or laser treatment. Used for precancerous changes.
- Excision (conization): Removes a small cone-shaped section of the cervix containing abnormal cells.
- Hysterectomy: Removes the uterus and cervix, sometimes advised for certain cancers or when other treatments aren’t suitable.
Chemotherapy
Uses medicines that travel through the bloodstream to destroy or slow cancer growth.
Chemotherapy may be:
- Given with radiation when cancer is local, or
- Used alone if cancer has spread or returned.
Common drugs include cisplatin, carboplatin, paclitaxel, docetaxel, topotecan, fluorouracil (5-FU), and bevacizumab.
Possible side effects: tiredness, nausea, hair loss, appetite loss, mouth sores, digestive changes, and menstrual changes like early menopause or reduced fertility.
Immunotherapy
Helps the immune system recognize and attack cancer cells. It’s mainly used when cervical cancer has spread or returned.
- Pembrolizumab (Keytruda): Given by IV every 3–6 weeks.
- Nivolumab (Opdivo): Given by IV every 2–4 weeks.
- Cemiplimab (Libtayo): Given by IV every 3 weeks.
Common side effects include fatigue, fever, nausea, rash, itching, and mild digestive or appetite changes.
Targeted Therapy
Targets specific molecules in cancer cells to slow growth or cause cell death. Used mainly for advanced or recurrent disease.
- Selpercatinib (Retevmo): For cancers with RET gene changes.
- NTRK inhibitors (larotrectinib, entrectinib): For cancers with NTRK mutations.
- Tisotumab vedotin: For advanced cervical cancer after chemotherapy.
- Fam-trastuzumab deruxtecan (Enhertu): For late-stage cases with specific HER2 involvement.
Each drug has distinct side effects, such as tiredness, nausea, liver test changes, or low blood counts, which are monitored closely by your care team.
Prevention
Cervical cancer prevention is highly effective because it focuses on stopping disease before it starts.
HPV vaccination is one of the biggest breakthroughs. Since most cervical cancers are caused by HPV, vaccination significantly lowers the risk of infection and long-term complications.
The vaccine works best when given before exposure to HPV, which is why it’s recommended for preteens but can also be given up to age 45.
Even with vaccination, screening is still essential. HPV vaccines don’t protect against all virus types linked to cervical cancer. Screening with Pap and/or HPV tests finds early, treatable changes before they progress.
- Get vaccinated against HPV (if eligible)
- Attend all routine cervical screenings
- Avoid smoking
- Practice safer sex
- Follow up promptly if screening tests show abnormal results
If glaucoma is already present, regular follow‑up visits are critical. Adjusting treatment early can prevent permanent vision loss. Many people maintain stable vision for years when eye pressure is well controlled—even without symptoms.
Related Topics
The Importance of Annual Well-Woman Visits
These yearly appointments are more than just routine checkups; they provide an opportunity to detect issues early, discuss changes in your body, and take control of your health.
The Importance of Annual Well-Woman Visits3 Cancers Every Woman Should Know
Cancer is one of the most pressing health concerns for women, yet some types develop silently, showing few warning signs until they’ve progressed. While screening and treatment have improved outcomes, awareness remains the first line of defense.
3 Cancers Every Woman Should Know