- Ectopic pregnancy occurs when a fertilized egg implants outside the uterus, most often in a fallopian tube, and cannot develop into a viable baby.
- Because the location cannot support growth, the condition can lead to rupture and life-threatening internal bleeding if left untreated.
- Symptoms include one-sided abdominal pain, vaginal bleeding, and shoulder pain; rupture causes severe pain and shock.
- Treatment may involve medication, surgery, or monitoring, depending on severity, with most people able to have healthy future pregnancies.
Overview
An ectopic pregnancy occurs when a fertilized egg implants and begins to grow outside the uterus, the normal site for fetal development. Since the fertilized egg cannot survive outside the uterus, an ectopic pregnancy is not viable and can become life-threatening, due to the risk of severe internal bleeding.
How an Ectopic Pregnancy Develops
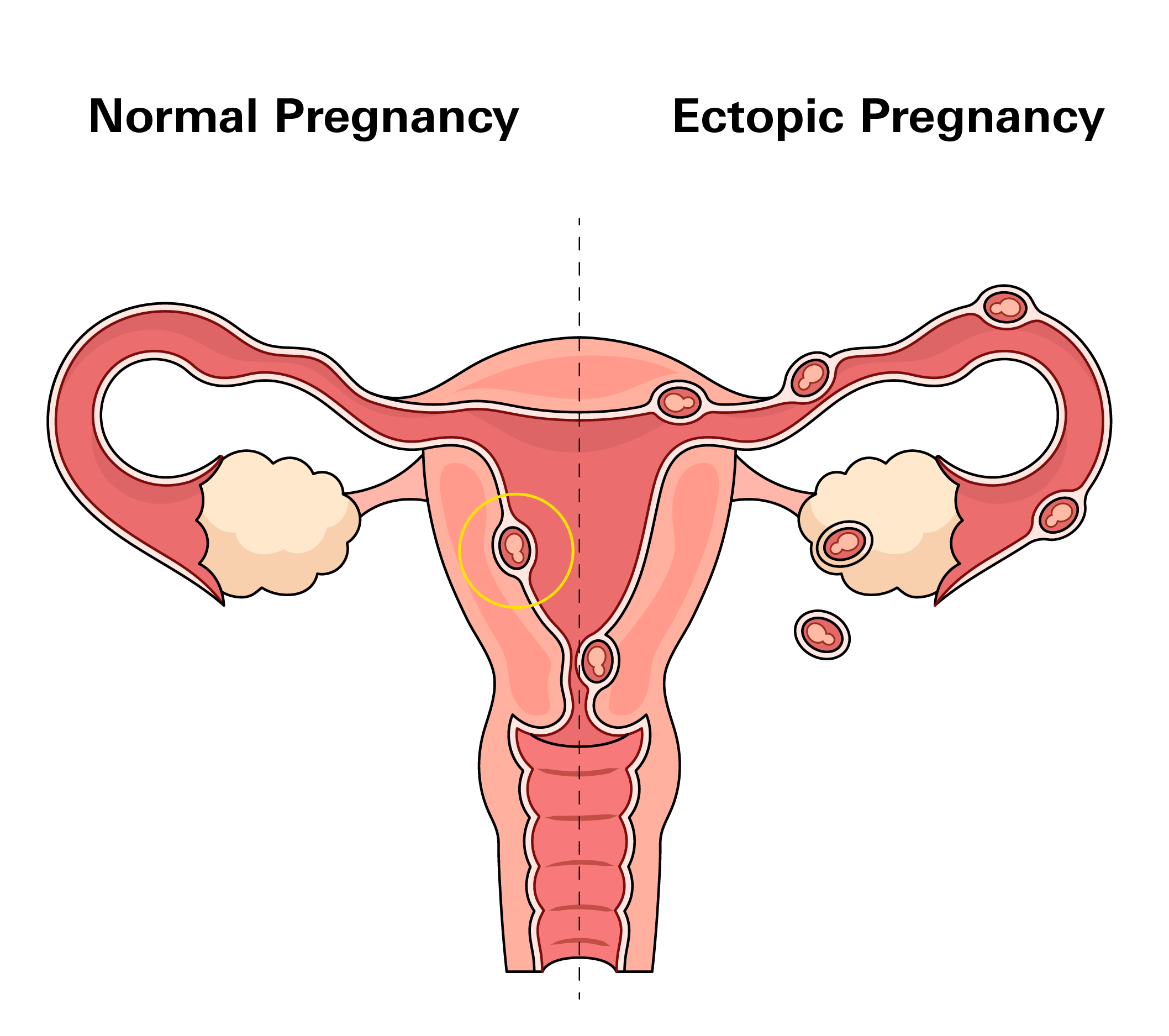
In a typical pregnancy:
- An ovary releases an egg
- Fertilization occurs in the fallopian tube
- The fertilized egg travels to the uterus and implants in its lining, where it can grow safely
In an ectopic pregnancy:
- The fertilized egg fails to reach the uterus
- It implants in a location that cannot support its growth, most often in a fallopian tube
- As the embryo grows, it can cause the tube to stretch, rupture, and bleed, leading to a medical emergency
How Common Is It?
This condition occurs in about 1% to 2% of all pregnancies in the United States. While this may seem rare, it accounts for tens of thousands of cases annually.
The risk is higher among people who conceive through fertility treatments, with about 2% to 5% of such pregnancies being ectopic. This increase is likely related to how eggs or embryos move through the fallopian tubes during assisted reproduction.
Types
Tubal Pregnancy
Approximately 95% of ectopic pregnancies are tubal (fallopian tube). It can implant in different parts of the tube:
- Ampullary (most common): Middle, widest section of the tube
- Isthmic: Narrow segment near the uterus
- Fimbrial: End closest to the ovary
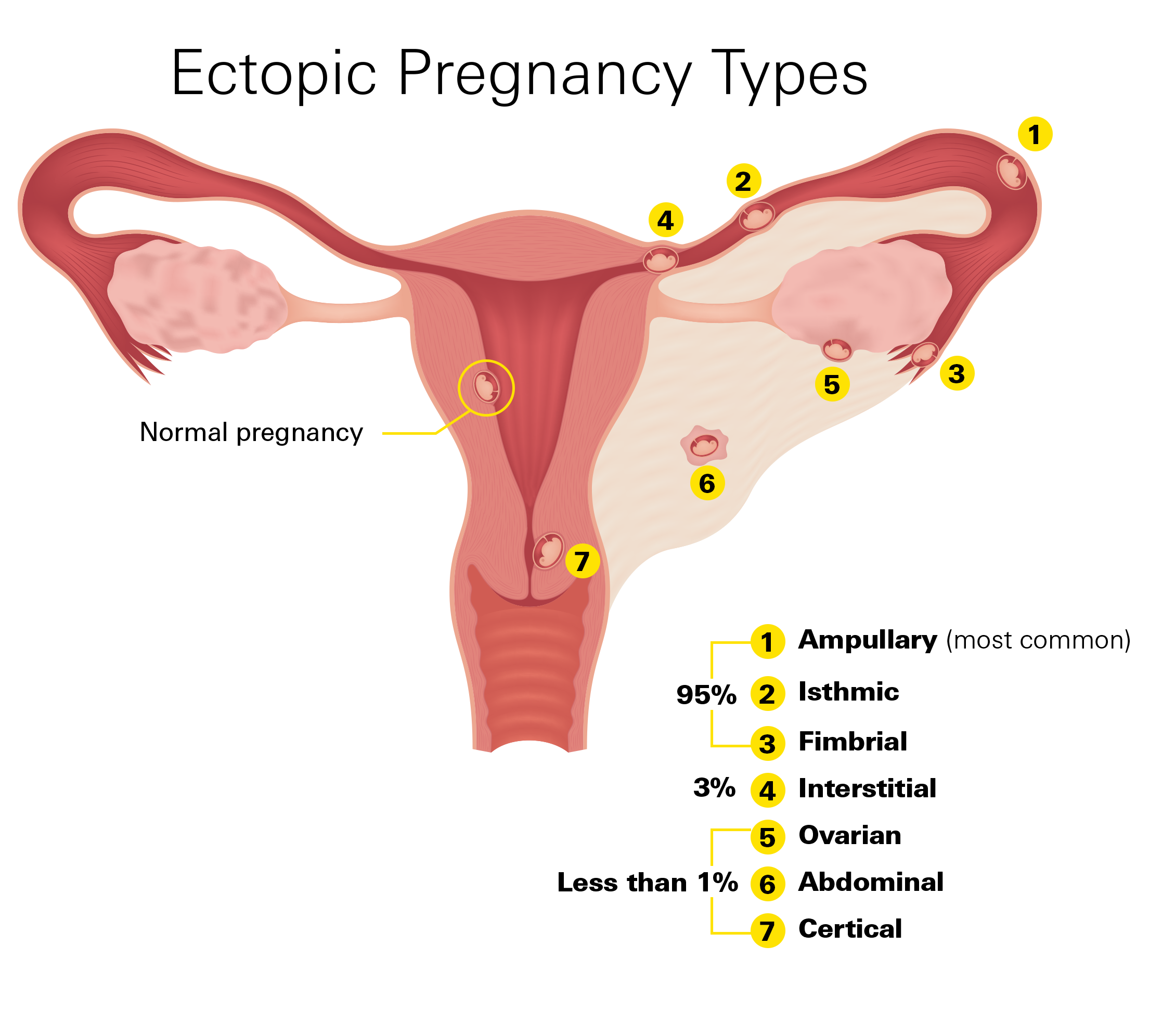
Interstitial Pregnancy
Interstitial (cornual) pregnancies (~3%) occur where the tube enters the uterine wally. This area has a rich blood supply, so rupture can cause heavy bleeding.
Rare Locations
Less than 1% occur in other unusual locations:
- Ovarian: Egg implants on or inside the ovary
- Cervical: Implants in the cervix, the lower part of the uterus
- Abdominal: Attaches to organs like the liver or intestines (extremely rare; may grow longer due to space. Very dangerous because the placenta may attach to vital organs, risking severe bleeding during removal.)
- Cesarean Scar: Grows within a previous surgical scar on the uterus
- Heterotopic: One embryo implants in the uterus and another outside it—more common with fertility treatments
Symptoms
An ectopic pregnancy typically develops within the first few weeks after conception, often before a missed period is noticed. Early hormonal changes mimic a normal pregnancy, making initial symptoms easy to overlook.
Early Signs (4–12 Weeks)
- Missed period and a positive pregnancy test
- Light vaginal bleeding, which may be lighter or darker than a regular period
- Mild cramping or pain on one side of the lower abdomen
- Nausea, bloating, or dizziness
- Shoulder or neck discomfort, which can result from internal bleeding irritating the diaphragm
Worsening Symptoms
As the pregnancy grows in an unsuitable location:
- Sharp or persistent abdominal pain, often focused on one side
- Heavier vaginal bleeding
- Pelvic pressure or discomfort
These signs suggest that the pregnancy is causing damage to surrounding tissues and may be approaching rupture.
Emergency Symptoms (Seek Immediate Care)
A ruptured ectopic pregnancy is a medical emergency. It can cause life-threatening internal bleeding and requires urgent treatment. Go to the hospital immediately if you experience:
- Sudden, severe abdominal or pelvic pain
- Dizziness, fainting, or rapid heartbeat
- Shoulder pain (a sign of internal bleeding affecting the diaphragm)
- Heavy vaginal bleeding or passing large clots
- Pale, sweaty skin or extreme weakness
Risk Factors
Ectopic pregnancy can happen to anyone, even without any known cause. However, several factors can increase the likelihood.
- Previous ectopic pregnancy: Recurrence risk is 10–15%.
- Fallopian tube damage: Surgery near the tubes (e.g., for cysts or infections) or conditions like pelvic inflammatory disease (PID) can cause scarring or narrowing, making it harder for the egg to reach the uterus.
- Infections such as chlamydia or gonorrhea can lead to inflammation and damage to reproductive organs.
Other known risk factors include:
- Becoming pregnant while using an intrauterine device (IUD). This is rare, but if pregnancy occurs, it is more likely to be ectopic.
- Undergoing fertility treatments. The risk rises to about 2% to 5%.
- Smoking, which affects how the tubes move the egg and increases ectopic risk up to fourfold.
- Being older than 35, as the fallopian tubes may not function as efficiently.
- Having structural differences in the uterus or fallopian tubes.
Importantly, about half of all ectopic pregnancies occur in people with no known risk factors. That is why recognizing early warning signs and seeking care promptly is so important.
Diagnosis
Early diagnosis is key to preventing complications. Because initial symptoms often resemble a normal pregnancy, many people don’t realize something is wrong until pain or bleeding worsens.
When an ectopic pregnancy is suspected, doctors typically start with:
- Blood tests to measure human chorionic gonadotropin (hCG). In a healthy pregnancy, hCG levels rise steadily. If they rise too slowly or begin to drop, it can signal a problem.
- Ultrasound, often transvaginal, to check whether a pregnancy is located inside the uterus. If no pregnancy appears in the uterus despite a high hCG level, it strongly suggests the pregnancy is growing elsewhere.
Sometimes results are unclear. In that case, your doctor may repeat blood and ultrasound tests over several days to track changes.
If there is still uncertainty and symptoms continue, a laparoscopy—a minimally invasive procedure using a thin camera—may be performed to look directly inside the abdomen and locate the pregnancy.
The main goal is to confirm the diagnosis before bleeding or rupture occurs.
Treatment
Treatment depends on the pregnancy’s location, size, and whether rupture has occurred. The goal is to resolve the pregnancy safely and prevent internal bleeding.
Medical Treatment (Methotrexate)
Used when the pregnancy is detected early and the fallopian tube has not ruptured. Methotrexate stops cell growth and allows the body to absorb the tissue.
It is given as an injection, usually in the arm or hip, followed by regular hCG monitoring. A steady drop means the medicine is working.
After the injection:
- Avoid alcohol, folic acid supplements, and NSAIDs (e.g., ibuprofen)
- Avoid sun exposure
- No sexual activity for 2 weeks
- Quit smoking
- Wait 3 months before trying to conceive again
Mild side effects such as abdominal cramping, light bleeding, or delayed periods are common and temporary. Grey-pink tissue discharge (uterine cast) can occur and is part of the healing process.
If hCG levels don’t drop sufficiently, a second dose may be needed. Weekly monitoring continues until levels reach zero.
Surgery
Surgery is required if internal bleeding has occurred, the fallopian tube has ruptured, or hormone levels are too high for medication to work safely.
- Laparoscopy: Minimally invasive surgery to remove the ectopic tissue and possibly the affected tube.
- Laparotomy: Open surgery used in emergencies with heavy bleeding.
Watchful Waiting
In rare cases, if the pregnancy is resolving naturally and hCG levels are falling, doctors may monitor without immediate intervention. It is only considered when there’s no pain, bleeding, or risk of rupture.
After Treatment
Regardless of the approach, close follow-up is critical. hCG levels are monitored until they return to zero to confirm that no pregnancy tissue remains.
It is also normal to discuss recovery and future fertility. Most people go on to have normal pregnancies afterward, though the risk of another ectopic pregnancy is slightly higher. For that reason, early ultrasound imaging is often recommended in future pregnancies to confirm implantation in the uterus.
Prevention
There is no guaranteed way to prevent an ectopic pregnancy. It can happen without warning and even in the absence of any known risk factors.
While addressing underlying issues may reduce the risk, no measures can fully eliminate it. The most effective safeguard is early evaluation. If you experience unexpected pain, bleeding, or dizziness in early pregnancy, contact your healthcare provider right away.
Early assessment cannot stop an ectopic pregnancy from developing, but it can help detect the problem before it becomes an emergency.
Related Articles
Navigating Fertility with Clomid
Clomid, or Clomiphene, is a medication used to help women who are having trouble getting pregnant due to issues like irregular periods or problems with ovulation. Read more on Clomid and Infertility
STI: All About Gonorrhea
Gonorrhea is a sexually transmitted infection (STI) caused by the bacterium Neisseria gonorrhoeae. It can affect both men and women and is transmitted through unprotected sexual contact, including vaginal, anal, and oral sex.
Read more about gonorrheaWhat to Know about Chlamydia
Chlamydia is one of the most common sexually transmitted infections (STIs) caused by the bacterium Chlamydia trachomatis. It can affect anyone who is sexually active, both men and women, and can infect various parts of the body.
Read more about chlamydiaMucinex and Fertility: What You Need to Know
Mucinex is an expectorant that thins mucus in the lungs and throat. Some people think it might do the same for cervical mucus, making it easier for sperm to move to the upper part of the female reproductive tract.
Read Mucinex for Infertility