- A sinus infection (sinusitis) is inflammation of the sinus cavities, often caused by viruses, bacteria, or allergies.
- Common symptoms include facial pressure, thick nasal discharge, headache, and reduced smell.
- Most infections are viral and improve without antibiotics, but longer or worsening symptoms may need them.
- Allergies, colds, smoking, and nasal problems increase the risk of sinus infections.
Overview
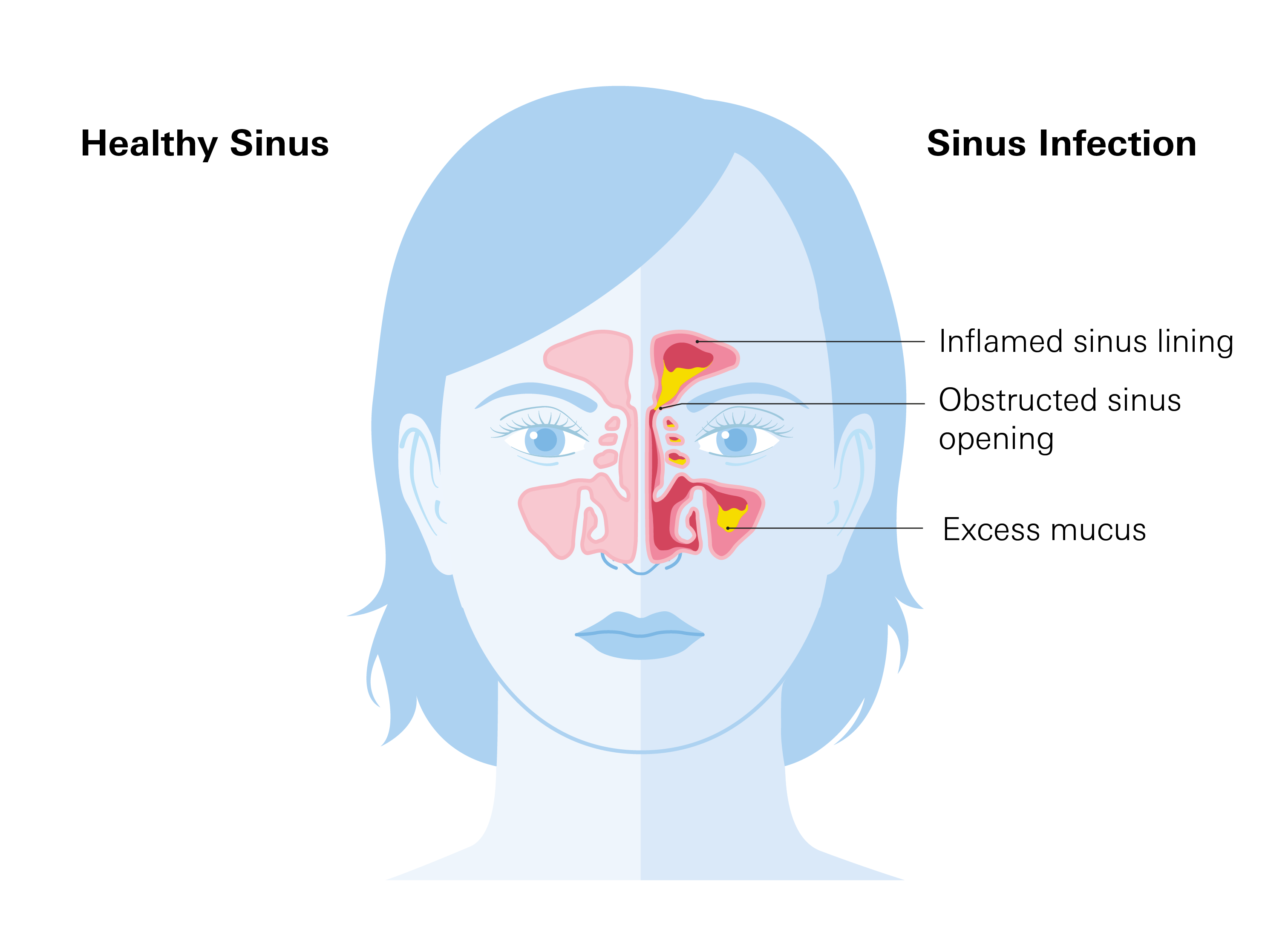
A sinus infection, also known as sinusitis, is an inflammation or swelling of the tissue lining the sinuses. Sinuses are the hollow, air-filled spaces located behind your forehead, cheeks, and eyes. They normally produce mucus that drains into your nose.
When these passages become blocked, mucus gets trapped, allowing germs to grow and cause an infection. Sinus infections are one of the most common health issues in the U.S., affecting millions of people each year and leading to numerous doctor visits and missed work or school days.
There are four main types:
- Acute: A sudden infection that lasts for up to 4 weeks. These are typically caused by a virus, like a common cold.
- Subacute: ymptoms persist for more than 4 weeks but less than 12 weeks.
- Chronic: An infection that continues for 12 weeks or longer, even with treatment. This type is often linked to allergies, nasal polyps, or ongoing irritation.
- Recurrent: Characterized by having four or more separate acute infections within one year, with symptom-free periods in between.
Sinus infections are a common health issue in the U.S., affecting millions annually. They are a leading cause of doctor visits and missed work or school days. Cases peak in fall and winter due to colds and flu, and in early spring for those with allergies.
Symptoms
The main signs of a sinus infection are facial pain and pressure. This pain is often felt across the forehead, cheeks, and around the eyes, and can worsen when you bend forward or lie down.
Unlike a regular cold, a sinus infection usually lasts longer and often presents with thick, discolored mucus.
Common symptoms include:
- Stuffy or runny nose with thick, often yellow or green mucus
- Headache and facial pain (forehead, cheeks, or behind the eyes)
- Postnasal drip and persistent cough
- Reduced sense of smell or taste
- Fever, fatigue, or bad breath in some cases
How to differenciate:
- Colds: Start with sneezing, sore throat, and clear mucus; typically resolve within a week.
- Allergies: Cause itching, watery eyes, and clear drainage without fever or facial pain.
- Sinus Infections: Last longer, produce thick mucus, and cause facial pressure.
Causes
Most sinus infections are viral, often starting as a common cold. The swelling from a cold blocks the sinus passages, trapping mucus and creating an ideal environment for germs to multiply.
Less commonly, sinus infections can be caused by bacteria or, in rare cases, fungi, particularly in people with weakened immune systems.
Risk Factors
Certain factors increase your risk of getting a sinus infection:
- Respiratory illnesses: Colds and other viruses are the most common trigger.
- Allergies: Conditions like hay fever can cause chronic inflammation and swelling in the nasal passages.
- Structural issues: Nasal polyps (small growths) or a deviated septum (a crooked wall between the nostrils) can block sinus drainage.
- Environmental factors: Exposure to cigarette smoke, air pollution, or dry indoor air can irritate the sinus lining.
- Weakened immune system: Conditions or medications that suppress your immune system make you more susceptible to infections.
Diagnosis
A healthcare provider can usually diagnose a sinus infection based on your symptoms and a physical exam. They will ask about the duration and type of your symptoms and may gently press on your face to check for tenderness. They may also look inside your nose with a light to check for swelling or discolored mucus.
For persistent or recurring infections, additional tests may be needed:
- Nasal endoscopy: A small, flexible tube with a camera is used to examine the nasal and sinus passages.
- CT scan: This imaging test provides a detailed view of the sinuses to identify blockages or other issues.
- Cultures: A sample of mucus may be tested to determine if bacteria or fungi are causing the infection, which helps guide treatment.
Treatment
Treatment for a sinus infection depends on its cause and duration. Since most infections are viral, they often get better on their own without antibiotics.
For Viral Sinus Infections
The goal is to relieve symptoms and promote drainage. You can use:
- Saline nasal sprays or rinses to keep passages moist and wash out mucus.
- Pain relievers like acetaminophen or ibuprofen for headaches and facial pain.
- Steroid nasal sprays (like fluticasone) to reduce swelling.
- Decongestants (like pseudoephedrine or oxymetazoline) to temporarily shrink swollen tissues and ease congestion. Note that nasal spray decongestants should only be used for a few days to avoid rebound congestion.
For Bacterial Sinus Infections
A doctor may prescribe antibiotics if symptoms last longer than 10 days, worsen after initially improving, or are severe from the start. Common antibiotics include amoxicillin or doxycycline. It's important to take the full course of antibiotics as prescribed, even if you start to feel better.
For chronic or recurrent infections, treatment may involve long-term medication use, allergy management, or procedures to open blocked sinuses and improve drainage.
Prevention
While not all sinus infections can be prevented, steps that lower the risk include:
- Wash your hands frequently to reduce the spread of viruses that can lead to a cold.
- Treat allergies to control inflammation and swelling in your nasal passages.
- Avoid cigarette smoke and air pollution, which irritate the sinuses.
- Stay up to date on vaccinations, especially for the flu and COVID-19, as these illnesses often precede a sinus infection.
- Avoid close contact with sick people, particularly during cold and flu season.
Related Topics
Allergy or Cold
Allergies are immune system responses to an allergen, such as pollen, dust, and/or pet dander, whereas colds are caused by viral infections in your upper respiratory tract.
Read moreAllergies, Cold, Flu, or COVID? How to Tell the Difference
Knowing the difference matters because treatments vary: antihistamines work for allergies, but they won’t help with the flu or COVID. And while colds usually just need rest and fluids, flu and COVID can sometimes require medical attention or prescription antivirals.
Read more