Why Lowering LDL Cholesterol Could Save Your Heart
- Lowering LDL (“bad”) cholesterol is one of the most powerful ways to prevent heart attacks and strokes.
- Long-term exposure to high LDL-C, especially early in life, causes gradual damage that increases cardiovascular risk as you age.
- Lifestyle changes help, but many people with high cholesterol or genetic risk also need medication to reach protective LDL-C levels.
- Common myths (e.g., “all cholesterol is bad,” “statins are more dangerous than high cholesterol,” “you’ll feel high cholesterol”) are incorrect and can delay life‑saving treatment.
Cholesterol is a naturally occurring substance that your body needs. It acts as a structural component for cell membranes and is essential for producing hormones (e.g., estrogen, testosterone), aiding in bile production for digestion, and helping the body produce vitamin D.
Your body makes most of its cholesterol, and it's not inherently harmful. Problems arise when levels get out of balance.
Cholesterol travels through your blood attached to lipoproteins. LDL ("bad") cholesterol carries cholesterol to your cells. When LDL is too high, it can deposit cholesterol in your artery walls, leading to plaque buildup.
How High LDL-C Contributes to Heart Disease
Elevated LDL-C allows excess cholesterol to seep into the lining of your arteries. Over time, this mixes with fats, calcium, and inflammatory cells to form plaque. Plaque narrows and stiffens arteries, restricting blood flow to vital organs like your heart and brain.
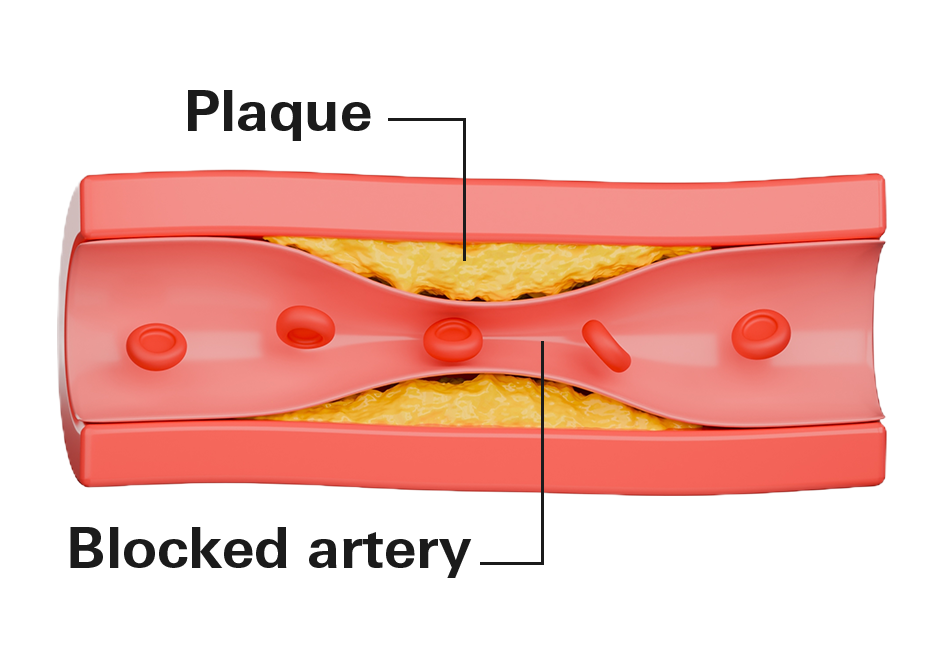
If plaque ruptures, it can trigger a blood clot that blocks an artery, causing a heart attack or stroke. This process often starts early in life and builds gradually, which is why managing LDL-C now is critical, even if you feel fine. 1 out of every 4 cardiovascular deaths is connected to long term exposure to high LDL cholesterol.
Common targets include:
- Around 100 mg/dL for adults without known heart disease
- Below 70 mg/dL for those with a history of heart attack or stroke on cholesterol meds
- Under 55 mg/dL for some high-risk patients
Reaching these often requires a combination of lifestyle changes and medication, especially if genetics play a role.
The dose–response is clear: lower LDL‑C → fewer events
Across hundreds of thousands of patients and many trials, every meaningful drop in LDL‑C cuts risk.
Key findings from studies:
- Every 1% drop in LDL cholesterol cuts heart disease and stroke risk by about 1%. The benefits can be bigger if starting LDL-C is high.
- Benefits persist even from already low baselines, like dropping from 70 mg/dL to 20 mg/dL, without safety trade-offs.
- People with higher LDL-C early in life face greater long-term risks, even if levels normalize later. Early intervention can prevent this cumulative damage.
- In older patients, lowering LDL-C still provides significant protection against events.
Why earlier control matters
Atherosclerosis builds slowly, often starting decades before symptoms. Cumulative LDL‑C exposure (how high for how many years) helps determine later risk. People who spend more years with high LDL‑C carry more plaque into midlife, even if their later LDL‑C matches someone else’s. Starting LDL‑C control earlier lowers lifetime event risk.
Lifestyle helps; medication is often required
Lifestyle changes are a strong starting point:
- Adopt a heart-healthy diet low in saturated fats and high in fruits, vegetables, whole grains, and lean proteins.
- Aim for regular physical activity, like 150 minutes of moderate exercise per week.
- Maintain a healthy weight, quit smoking, and manage stress.
However, genetics and biology often limit how far lifestyle alone can move LDL‑C. That’s why guidelines recommend statins as first‑line therapy for many patients.
- High‑intensity statins typically lower LDL‑C by 50% or more; moderate intensity by 30–49%. Bigger LDL‑C drops translate into bigger risk reductions.
- When LDL‑C remains above goal (e.g., >70 mg/dL in very‑high‑risk ASCVD), adding ezetimibe and then a PCSK9 inhibitor is recommended.
Safety and balance
It’s reasonable to ask about side effects. In blinded randomized trials muscle aches appear with similar frequency on placebo and statins (5–12%), and serious complications are uncommon. Importantly, avoiding statins when indicated raises the risk of preventable heart attacks and strokes.
The very‑low LDL‑C data are also reassuring: meta‑analyses and outcomes trials that pushed LDL‑C to <25 mg/dL did not show signals for cancer, hemorrhagic stroke, liver or muscle injury, or cognitive decline over trial durations.
Common cholesterol myths
Lowering LDL‑C is one of the strongest, most proven ways to protect your heart. But when it comes to cholesterol, misunderstandings are everywhere. Many can delay or derail effective treatment. Let’s clear up the most common myths.
Myth 1: All cholesterol is bad
Cholesterol is essential for normal body function. The danger lies in the balance of lipoproteins. While high levels of LDL contribute to plaque buildup, HDL (High-Density Lipoprotein) is generally linked to lower cardiovascular risk. The goal of treatment is to manage the specific particles that cause harm.
Myth 2: You can feel high cholesterol
High cholesterol is a "silent" condition. Plaque can build up in your blood vessels for decades without a single warning sign. Most people do not experience symptoms like chest pain until an artery is already significantly blocked or a heart attack occurs. Regular testing is the only way to identify risk before a crisis.
Myth 3: Eating foods high in cholesterol (like eggs, shrimp, or organ meats) directly raises your blood cholesterol
For most people, dietary cholesterol has only a modest effect on blood levels because your liver produces the majority (~80%) of your body's cholesterol. Saturated and trans fats have a much stronger impact on raising LDL.
Foods like eggs and shrimp are high in cholesterol but low in saturated fat, and do not significantly increase heart disease risk.
Myth 4: Saturated fat has been exonerated; it doesn’t affect heart risk
Saturated fat clearly raises LDL cholesterol and is a major pathway to higher ASCVD risk. Claims that saturated fat is “harmless” often cherry-pick studies or ignore the replacement nutrient (e.g., refined carbs versus unsaturated fats).
Large reviews conclude that replacing saturated fat with polyunsaturated fat lowers ASCVD risk; simply swapping saturated fat for refined carbohydrates does not provide the same benefit.
Myth 5: Statins are more dangerous than high cholesterol itself
Statins are among the most studied and safest medications. Statins significantly lower LDL and reduce heart attack and stroke risk. Social media exaggerates side effects; controlled studies show muscle-related symptoms occur in 5–12% of both placebo and statin groups, indicating perception bias.
Avoiding statins raises risk of preventable cardiovascular events.
Myth 6: Diet and exercise alone determine your cholesterol levels
Conditions like familial hypercholesterolemia cause very high LDL regardless of diet. Lifestyle is important, but not the sole determinant, genetics, inflammation, insulin resistance, and age all play significant roles.
Myth 7: Seed oils (like canola, sunflower, soybean) are toxic, cause inflammation, or are the real driver of heart disease (while saturated fats/animal fats are harmless or beneficial)
Decades of research show replacing saturated fats with unsaturated fats (including those from most seed oils) lowers LDL cholesterol and reduces cardiovascular risk. Claims demonizing seed oils often ignore this evidence or rely on outdated/animal studies. Saturated fats (from butter, red meat, etc.) remain more concerning for raising LDL.
Myth 8: Extreme low-carb or carnivore diets fix cholesterol issues and prove LDL/high cholesterol isn't harmful
These diets can raise LDL significantly in many people due to high saturated fat intake. While some markers may improve short-term, long-term evidence doesn't support ignoring elevated LDL, and mainstream guidelines still link high LDL to increased atherosclerotic cardiovascular disease risk.