- Gout is a type of arthritis caused by high uric acid levels, leading to painful joint inflammation, often in the big toe.
- Symptoms include sudden, intense joint pain, swelling, redness, and warmth, typically during nighttime flare-ups.
- Risk factors include diet, obesity, certain medical conditions, genetics, and dehydration, with men more commonly affected.
- Treatment includes anti-inflammatory medications for flares and long-term drugs to lower uric acid, along with lifestyle changes for prevention.
Overview
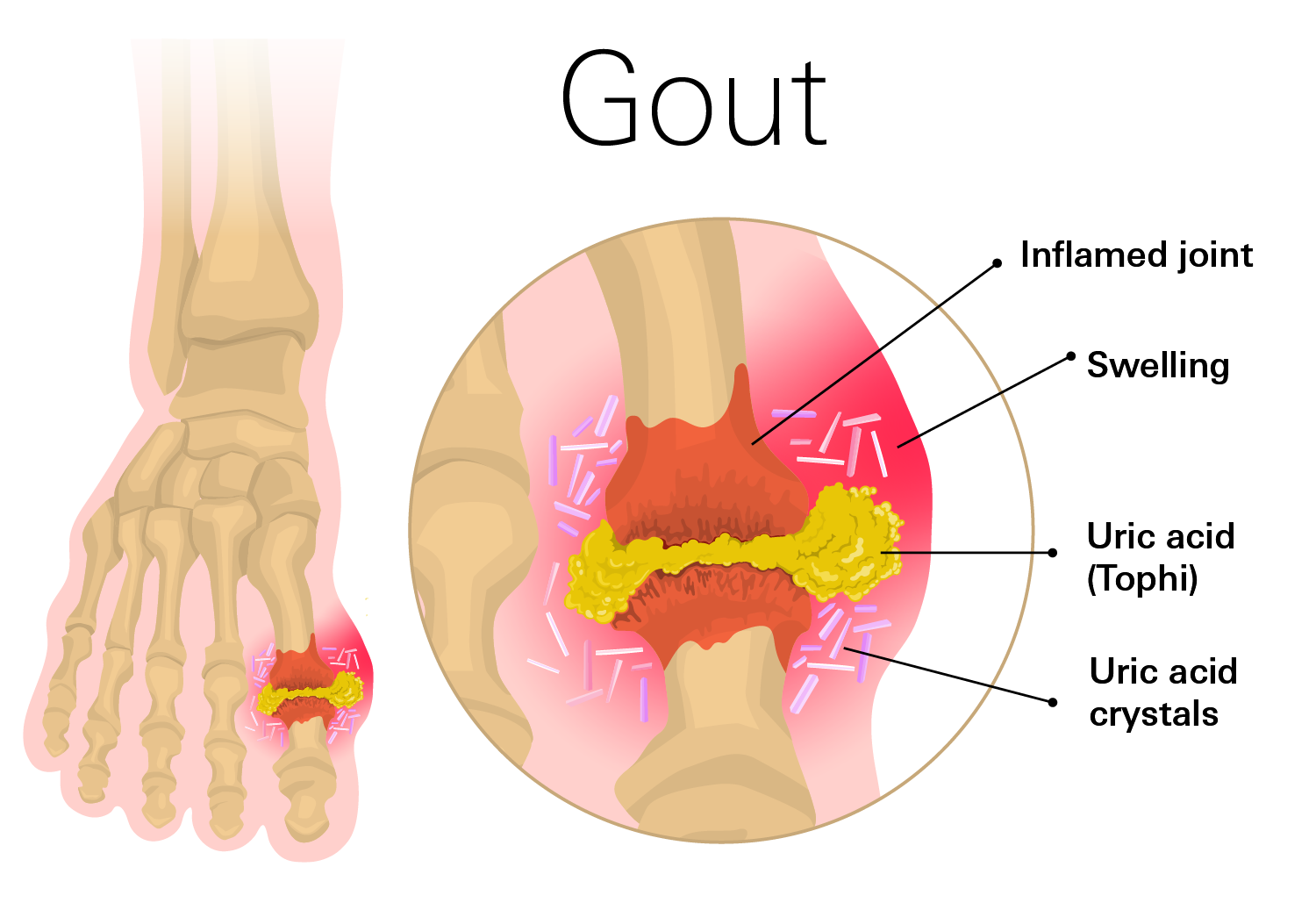
Gout is a common type of inflammatory arthritis that causes sudden, intense episodes of joint pain and swelling. It most often affects the big toe but can occur in any joint, including ankles, knees, elbows, wrists, or fingers. These attacks, or flare-ups, are triggered by high levels of uric acid in the blood (hyperuricemia), which can form sharp, needle-like crystals in the joints.

Normally, uric acid — a waste product from breaking down natural substances called purines — dissolves in the blood, passes through the kidneys, and is excreted in urine. When the body produces too much or the kidneys cannot remove enough, uric acid builds up. This can lead to gout attacks and, over time, permanent joint damage if untreated.
Gout symptoms include intense joint pain, swelling, redness, warmth, and tenderness that often start suddenly, especially at night, and can last for days to weeks. These flares may come and go, but without management, they can become more frequent and lead to long-term joint damage.G
How common is it?
According to the CDC, gout affects about 4% of U.S. adults, or roughly 8 million people. It is more common in men, who often develop symptoms between ages 30 and 50. In women, risk increases after menopause due to lower estrogen levels. Rates have risen in recent decades, partly due to diet, obesity, and an aging population.
Symptoms
Gout symptoms often appear suddenly and can be extremely painful, typically affecting one joint at a time during a flare-up, though multiple joints may be involved over time. Flares often start at night and can wake you from sleep.
Common symptoms include:
- Intense joint pain, most often in the big toe, but also possibly in the ankles, knees, elbows, wrists, or fingers. The pain is usually worst within the first 4 to 12 hours.
- Swelling in the affected joint.
- Redness and warmth around the joint.
- Tenderness, where even light pressure (like from a bedsheet) can be unbearable.
- Limited range of motion in the joint.
- Lingering discomfort that may last days to weeks.
- Chest pain that is severe or worsening
- Tophi, which are hard lumps under the skin around joints, tendons, or other areas in advanced cases. These can become swollen and painful during flares.
Stages of Gout
Gout progresses through four distinct stages:
- Asymptomatic hyperuricemia: Your blood uric acid levels are high, but you have no symptoms. Crystals may begin forming in joints, but you might not notice. This stage can last for years, and lifestyle changes can help prevent progression.
- Acute gout: Sudden attacks start, causing intense pain, swelling, redness, and warmth in a joint, often the big toe. Flares typically last days to weeks and then fully resolve. These are triggered by uric acid crystals causing inflammation.
- Intercritical (interval) gout: This is the period between flares when you feel normal and have no symptoms, but uric acid levels remain high. Without treatment, flares are likely to return, becoming more frequent and severe.
- Chronic tophaceous gout: In this advanced stage, repeated flares lead to ongoing crystal buildup, forming tophi—hard, lumpy deposits under the skin around joints, tendons, or even ears. Tophi can cause permanent joint damage, deformities, reduced mobility, and complications like kidney stones. This stage usually develops after years of untreated gout.
Causes
Gout happens when uric acid builds up in the blood and forms crystals in the joints. This may result from:
- The body producing too much uric acid
- The kidneys not removing enough uric acid through urine
Purines — found in certain foods, drinks, and naturally in the body — break down into uric acid. High intake of purine-rich foods (like some meats and seafood) and alcohol can raise uric acid levels.
Not everyone with high uric acid levels develops gout, but persistent high levels increase the risk of crystals forming and triggering attacks. Both genetics and lifestyle factors play a role in why this buildup happens.
Risk Factors
- Diet: Eating large amounts of red meat, organ meats, shellfish, alcohol (especially beer), and sugary drinks.
- Obesity: Higher body weight increases uric acid production and reduces clearance.
- Medical conditions: Hypertension, diabetes, kidney disease, and some metabolic disorders.
- Age and gender: More common in men ages 30–50; risk in women rises after menopause.
- Family history: A genetic tendency for high uric acid levels.
- Dehydration: Less uric acid is excreted when the body lacks fluids.
- Recent surgery or injury: Physical stress can trigger a flare-up if uric acid is high.
Complications
If left untreated, gout can lead to serious health issues:
- Joint damage: Repeated flares can cause chronic arthritis and permanent joint changes.
- Tophi formation: Hard uric acid deposits under the skin can become painful and deform joints.
- Kidney stones: Uric acid crystals may form in the kidneys, causing pain and potential damage.
- Kidney disease: Gout increases the risk of chronic kidney disease and, in severe cases, kidney failure.
Diagnosis
Diagnosing gout typically begins with a review of your symptoms, including joint pain patterns, swelling, and redness. Your doctor may also ask about your diet, medications, and family history of gout or related conditions.
To confirm the diagnosis, your doctor may recommend several tests:
- Joint fluid analysis: A small sample of fluid is drawn from the affected joint using a needle. When examined under a microscope, the presence of needle-shaped uric acid crystals confirms gout. This is the most definitive test.
- Blood tests: These measure uric acid levels in your blood. High levels (hyperuricemia) can suggest gout, but they’re not conclusive, as some people with high uric acid don’t develop gout, and others with normal levels may have flares.
Imaging tests:
- X-rays: Help rule out other joint conditions.
- Ultrasound: Detects uric acid crystals in joints or soft tissues.
- Dual-energy CT scans: Can identify uric acid deposits even in early stages.
Treatment
Gout treatment focuses on two main goals: relieving pain during flares and preventing future attacks by managing uric acid levels.
Treating Acute Gout Attacks
These medications help reduce inflammation and pain during a flare:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Ibuprofen (Advil, Motrin), Naproxen (Aleve), Indomethacin.
Side effects: Stomach upset, nausea, ulcers, kidney issues - Colchicine: Reduces inflammation from uric acid crystals. Most effective when taken early.
Side effects: Diarrhea, nausea, abdominal cramps. - Corticosteroids: If NSAIDs or colchicine aren’t suitable (e.g., due to kidney issues or allergies), corticosteroids like prednisone can reduce inflammation and pain. They may be given as pills or injections.
Side effects: Mood changes, increased appetite, elevated blood sugar, weight gain.
Long-Term Management
After the acute attack resolves, treatment shifts to lowering uric acid levels and preventing recurrence or joint damage.
- Xanthine oxidase inhibitors: Medications like allopurinol or febuxostat reduce the body’s production of uric acid, helping prevent crystal formation.
Side effects: Skin rash, upset stomach, liver function changes. - Uricosurics (e.g., probenecid): These help your kidneys remove uric acid more effectively, lowering blood levels.
Side effects: Nausea, joint pain, chest discomfort - Uricase (for severe cases):Converts uric acid into a form that’s easier to eliminate. Used when other treatments fail.
Prevention
Preventing gout involves a combination of lifestyle changes and, when needed, medications to manage uric acid levels.
Lifestyle Strategies
- Eat a balanced, low-purine diet: Limit foods high in purines, such as red meat, organ meats (like liver), shellfish, and certain fish (e.g., sardines, anchovies). Cut back on alcohol, especially beer. Focus on low-purine foods like vegetables, fruits, whole grains, and low-fat dairy.
- Stay hydrated: Drink plenty of water to help your kidneys flush out uric acid. Aim for 8–12 cups daily, unless your doctor advises otherwise.
- Maintain a healthy weight: Losing excess weight can lower uric acid production and ease stress on your joints.
- Limit sugary drinks and foods: Especially those with high-fructose corn syrup.
- Exercise regularly: SAim for at least 150 minutes of moderate activity per week.
Medical Monitoring
If you’ve had frequent flares or have a history of gout, talk to your doctor about:
- Regular blood tests to monitor uric acid
- Medication options for long-term control
- Personalized dietary and lifestyle recommendations
Related Topics
Top 9 Drugs To Combat Gout
Gout is a form of arthritis caused by the crystallization of uric acid (UA) in your joints. Uric acid is a byproduct of purine metabolism. One of the base pairs of DNA is made up of purines, which are found in many foods.
Read more