- Hemorrhoids are swollen veins in the lower rectum or around the anus. Internal hemorrhoids form inside the rectum, often painless but may bleed. External hemorrhoids form under the anal skin, typically causing pain and itching.
- They are very common, affecting about 50% of adults, and are primarily caused by increased pressure from straining during bowel movements, chronic constipation, prolonged sitting, or pregnancy.
- Most cases improve with fiber, hydration, and over-the-counter treatments; severe cases may need medical procedures.
Overview
A hemorrhoid is a swollen or inflamed vein n the lower rectum or around the anus. These veins are a normal part of the body's anatomy, acting as cushions that help control the passage of stool. They become problematic when increased pressure causes the vein walls to stretch, bulge, and become irritated, which can cause discomfort, pain, or bleeding.
How Common Is It?
Hemorrhoids are one of the most common digestive conditions among adults.
- Approximately 50% of adults will experience hemorrhoids at least once in their lifetime, especially after the age of 40.
- In any given year, about 5% of adults has noticeable symptoms like bleeding, swelling, or itching.
- Both men and women are affected equally, though pregnancy and childbirth significantly increase the risk for women.
Symptoms
Symptoms vary by hemorrhoid type and severity, ranging from mild itching to significant pain or bleeding. Most cases improve with self-care, but severe symptoms require prompt medical attention.
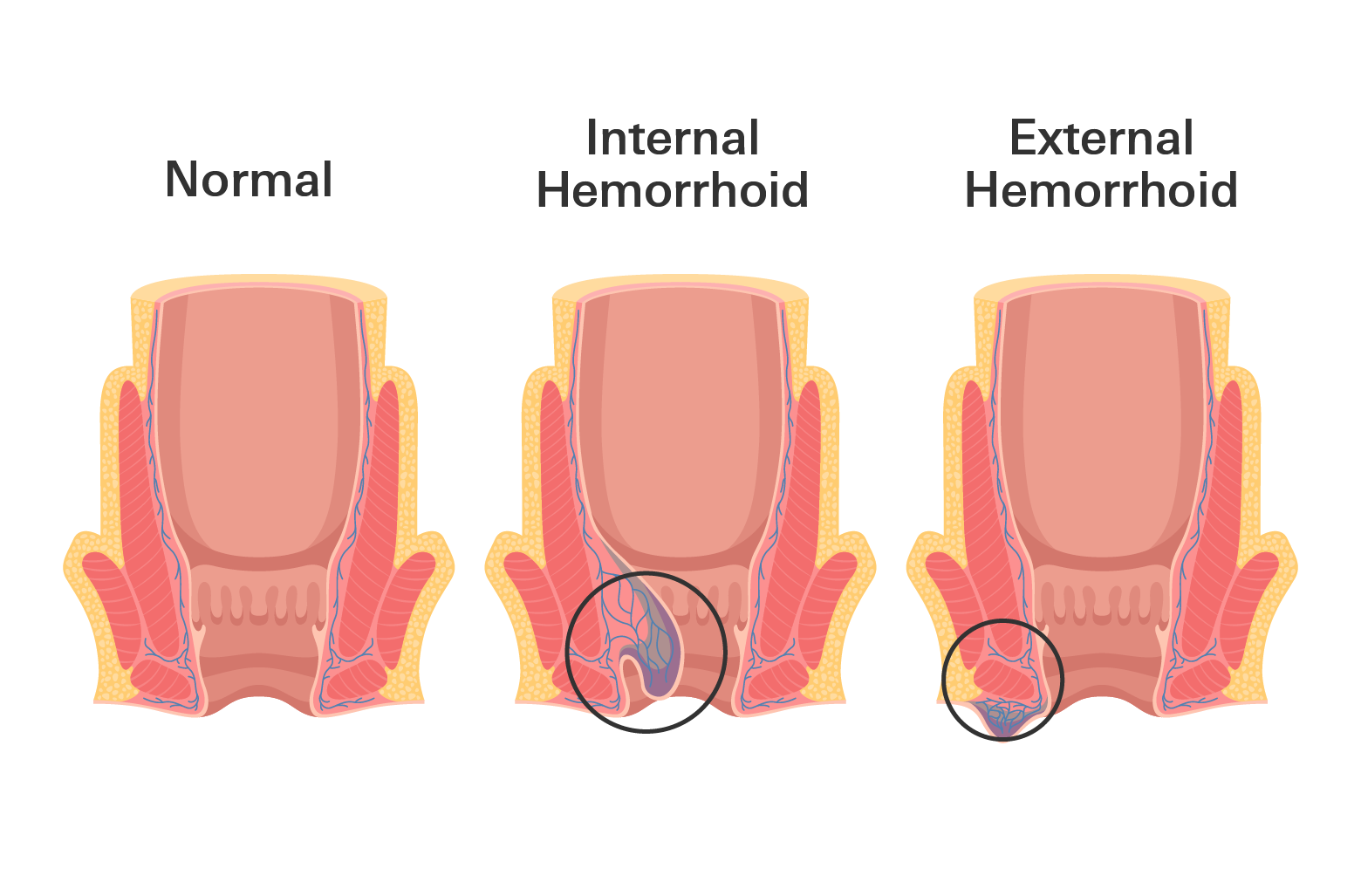
Internal Hemorrhoids
Form inside the rectum, above the anal opening; often painless due to fewer nerves.
- Bright red blood on toilet paper, in the toilet, or on stool
- Feeling of pressure or fullness in the rectum
- Prolapse (soft tissue bulging through the anus during bowel movements, which may retract on its own)
External Hemorrhoids
Form under the skin around the anus; painful due to many nerves.
- Pain, tenderness, or throbbing, especially when sitting, wiping, or during bowel movements
- Itching, irritation, or burning around the anus
- Swelling or a hard lump near the anal opening
- Minor bleeding
When to Seek Medical Attention
Most hemorrhoids are not dangerous and improve with care. But sometimes, the swelling or bleeding can become more serious and require medical attention.
- Heavy, continuous bleeding that lasts more than a few days
- Dark, black, or tar-colored stool
- Sharp or constant pain that doesn’t ease with home care
- Swelling that grows quickly or makes it hard to walk or sit
- Fever, drainage, or redness that spreads around the anus
- Lightheadedness, weakness, or fainting after bleeding
These symptoms could point to a clot, significant blood loss, or an infection that needs treatment.
Causes
Hemorrhoids develop when pressure increases in the lower rectum, causing veins to stretch and swell. Common triggers include straining, prolonged sitting, or sudden pressure increases. Supporting tissues naturally weaken with age, making veins more prone to bulging.
Common Causes and Risk Factors
- Chronic constipation or straining during bowel movements (most common; often due to low-fiber diets)
- Prolonged sitting, especially on the toilet
- Chronic diarrhea (frequent irritation inflames veins)
- Pregnancy and vaginal childbirth (uterine pressure and straining)
- Obesity (extra weight increases abdominal pressure)
- Heavy lifting or intense straining without core support
- Aging (tissues lose elasticity after age 40–50)
- Low-fiber diet (leads to hard stools and straining)
- Family history
- Sedentary lifestyle
Multiple overlapping factors heighten risk; for example, constipation combined with obesity or pregnancy markedly increases likelihood.
Diagnosis
Hemorrhoids are typically diagnosed during a quick office visit with a primary care doctor. If symptoms persist, recur, or are complex, referral to a gastroenterologist or colorectal surgeon may be needed for advanced evaluation.
Diagnostic Methods
- Visual Exam: The doctor inspects the area around the anus for signs of external hemorrhoids, such as swelling, lumps, or irritation.
- Digital Rectal Exam: A gloved, lubricated finger is gently inserted into the rectum to check for internal swelling, tenderness, or abnormalities.
- Anoscopy: A short, lighted tube (anoscope) is used to view the lining of the anus and lower rectum, helping confirm internal hemorrhoids or sources of bleeding.
- Rigid Proctosigmoidoscopy: This test uses a firm, lighted scope to examine the rectum and lower colon, especially if bleeding is ongoing or the diagnosis is unclear.
- Colonoscopy: If you're over 40 or have heavy or unexplained bleeding, a full colonoscopy may be done to rule out other conditions like colorectal cancer.
These procedures are usually quick, done in-office, and rarely require anesthesia.
Treatment
Treatment depends on symptom severity, duration, and hemorrhoid type. Most cases resolve with conservative measures; persistent or severe cases may require procedures.
At-Home Care
- Increase fiber and fluids: Consume high-fiber foods (fruits, vegetables, whole grains) and drink 8–10 glasses of water daily to soften stool and reduce straining.Increase fiber and fluids: Consume high-fiber foods (fruits, vegetables, whole grains) and drink 8–10 glasses of water daily to soften stool and reduce straining.
- Sitz baths: Soak in warm water for 10–15 minutes, 2–3 times daily, to ease pain and swelling.
- Cold compresses: Apply ice wrapped in cloth for 10 minutes to reduce acute swelling.
- Avoid prolonged sitting, especially on the toilet; limit to 5 minutes per session.
Over-the-Counter (OTC) Treatments
- Topical hemorrhoid creams/ointments (e.g., Preparation H): Contain phenylephrine to shrink tissue or witch hazel/aloe to soothe irritation.
- Medicated wipes/pads (e.g., Tucks): Provide witch hazel–based relief for itching and discomfort.
- Hydrocortisone cream (1%): Reduces inflammation and itching (use sparingly, max 7 days).
- Stool softeners (e.g., docusate/Colace): Prevent hard stools without stimulating bowels.
- Oral pain relievers: Acetaminophen, ibuprofen, or naproxen for discomfort (follow dosing instructions).
Medical Procedures
If symptoms do not improve after a week or two of self-care, or if bleeding is frequent, a doctor may recommend an in-office procedure:
- Rubber Band Ligation: A small rubber band is placed around the base of the internal hemorrhoid, cutting off its blood supply. The hemorrhoid then shrinks and falls off within a week (effective for internal grades 1–3).
- Sclerotherapy: A chemical solution is injected into the hemorrhoid, causing it to shrink and scar.
- Infrared Coagulation (IRC): Heat or light is used to seal off the blood vessel feeding the hemorrhoid, causing it to wither.
- Surgical Treatments (for severe cases):
- Hemorrhoidectomy: Surgical removal of large or severe hemorrhoids (outpatient, full recovery in 2–4 weeks).
- Stapled Hemorrhoidopexy: A surgical method that uses staples to reposition prolapsed internal hemorrhoids and restrict blood flow to the area (less pain than traditional surgery).
Prevention
Hemorrhoids are largely preventable with consistent lifestyle habits that reduce rectal pressure and straining.
- Don’t Delay Bowel Movements: Go when you feel the urge to avoid hard stools and straining.
- Limit Time on the Toilet: Avoid reading or using your phone while seated, as this increases pressure on rectal veins.
- Eat a High-Fiber Diet (25–35 g/day): Include plenty of fruits, vegetables, legumes, and whole grains.
- Stay Hydrated: Drink enough water to help fiber work effectively.
- Exercise Regularly: Physical activity promotes healthy digestion and reduces constipation.
- Avoid Heavy Lifting: Or use proper technique to reduce abdominal pressure.
- Manage Stress: Chronic stress can affect digestion and bowel habits.
Related Topics
What Can You Do About Hemorrhoids?
Hemorrhoids are an uncomfortable condition that effects almost half the population at some point by the age of 50. Hemorrhoids are characterized by bulging swollen blood vessels in and/or around your anus and can be very uncomfortable.
Top OTC Medications for Hemorrhoid Relief
Hemorrhoid creams and ointments are among the most popular OTC treatments. They work by soothing the irritated area, reducing inflammation, and protecting the skin from further irritation.
Top OTC products for hemorrhoids