- Meningitis is inflammation of the brain and spinal cord coverings, most often caused by viruses (common, usually mild) or bacteria (less common but dangerous).
- The most recognizable symptoms are a sudden high fever, a severe headache, and a painfully stiff neck.
- It spreads through close contact, respiratory droplets, and shared items depending on the cause.
- Bacterial meningitis requires emergency antibiotics; vaccines significantly reduce the risk of several major types.
Overview
Meningitis is the inflammation of the meninges, the protective membranes that surround your brain and spinal cord. When these layers swell, usually due to an infection, it can interfere with normal brain function and create a medical emergency.
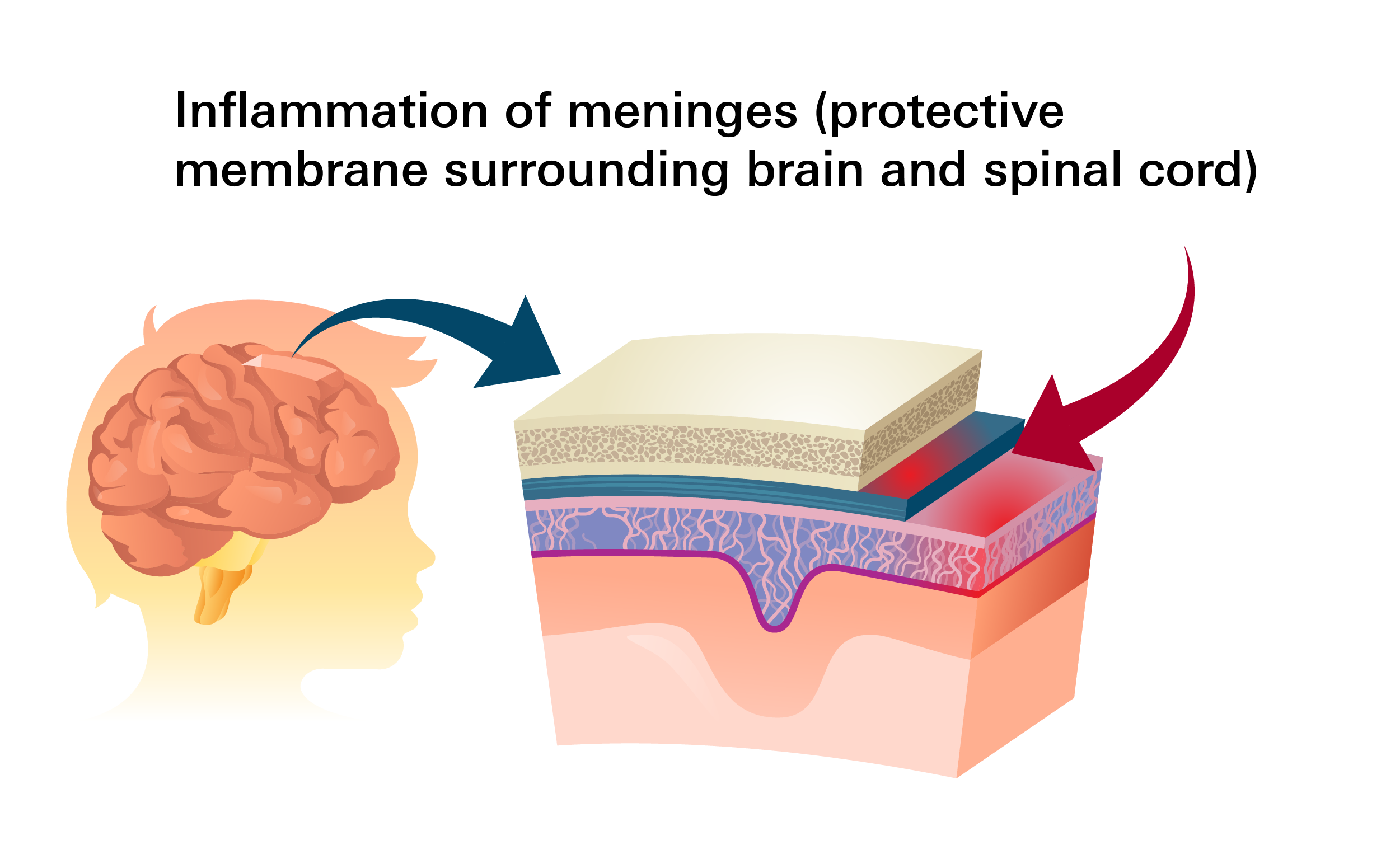
Because the swelling occurs so close to the central nervous system, meningitis can be life-threatening, especially bacterial forms, as swelling may impair brain function and lead to complications like hearing loss, seizures, or death if untreated.
The severity depends largely on the cause. Some types (mainly bacterial and certain viral) are contagious via respiratory droplets, saliva, coughing, sneezing, or shared items like utensils.
How common is it?
Meningitis is uncommon but still affects several thousand people in the United States each year.
- Viral meningitis is the most common form. Bacterial meningitis occurs less frequently but is responsible for the majority of serious complications and deaths.
- It spreads more easily in "congregate" or shared living settings, such as college dormitories, military barracks, and nursing homes.
- Infants are at high risk due to developing immune systems. Teenagers and young adults see higher rates due to social behaviors and living environments.
Types & Causes
Meningitis is classified by cause, with viruses and bacteria responsible for most cases.
Viral meningitis (most common)
Caused by many everyday viruses that reach the tissues around the brain and spinal cord. This type often clears up without specific medical treatment in people with healthy immune systems, though infants, older adults, and people with weakened immune systems may need hospital care.
- Common causes: Non-polio enteroviruses (most common), West Nile virus, Herpes simplex, Epstein‑Barr virus, Varicella‑zoster virus (chickenpox/shingles virus), the Influenza virus
- How it spreads: Through direct contact with saliva, respiratory secretions, or contaminated surfaces.
Bacterial meningitis (less common, more severe)
This is a severe, rapidly progressing form of the disease. It occurs when bacteria invade the bloodstream and travel to the brain. Without treatment, it can be fatal.
- Common causes: Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Group B Streptococcus, Listeria monocytogenes, Escherichia coli
- How it spreads: Through close or prolonged contact, such as kissing, coughing, or sharing utensils.
Early antibiotic therapy is critical. Without prompt care, bacterial meningitis can cause permanent damage or be fatal.
Symptoms
Symptoms can appear suddenly. While viral and bacterial meningitis share some "classic" signs, bacterial meningitis symptoms are typically more intense and worsen rapidly.
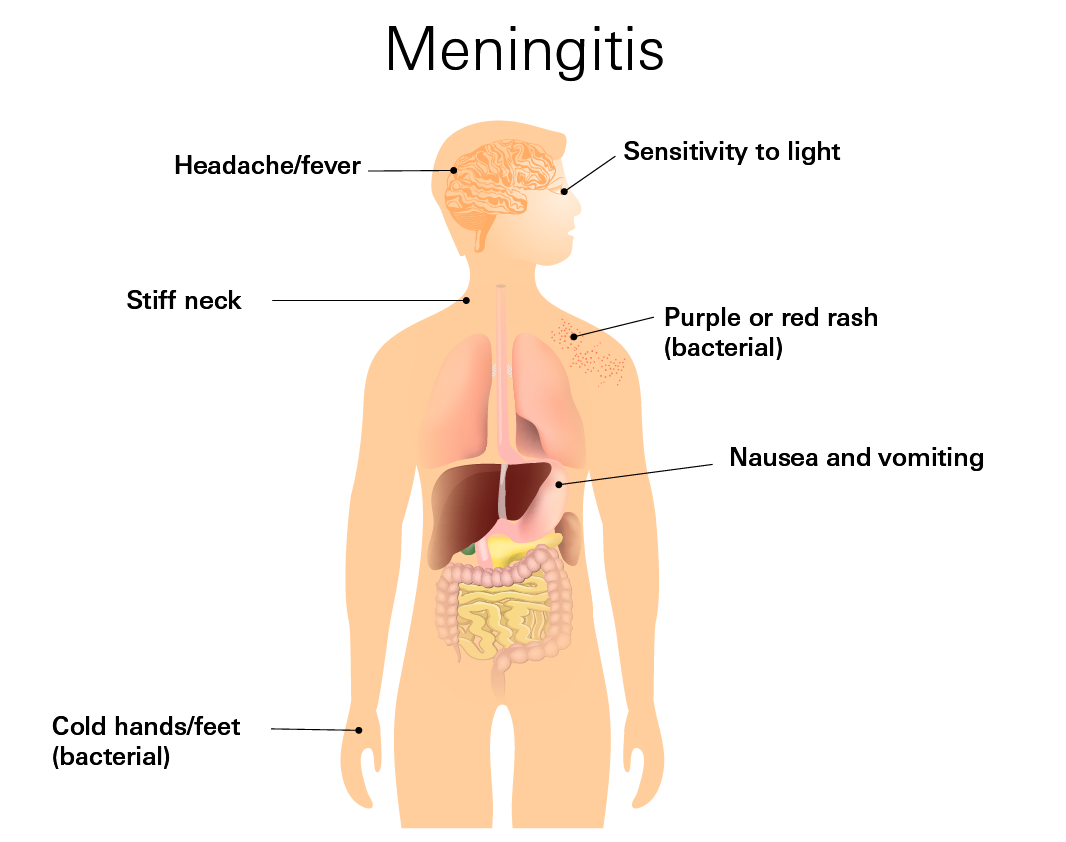
Common symtoms (both types)
- Fever
- Headache
- Stiff neck
- Sensitivity to light
- Nausea or vomiting
- Fatigue or body aches
Symptoms in infants
Infants may not show a stiff neck. Instead, look for:
- A bulging "soft spot" (fontanel) on the top of the head
- Constant crying or extreme irritability
- Poor feeding or vomiting
Bacterial (severe) infection
- Confusion or altered mental state
- Seizures
- Dark purple or red spots on the skin that do not fade when pressed
- Cold hands and feet with a mottled (blotchy) skin appearance
When to go to the hostpidal
Meningitis can progress with terrifying speed. Do not wait for all symptoms to appear. Seek immediate hospital care if you or someone else experiences:
- High fever and a stiff neck
- Sudden confusion or inability to wake up
- A severe headache that feels "out of the ordinary"
- Rapidly spreading purple or red spots on the skin
Risk Factors
Bacterial risk factors:
- Missing vaccines: Not being up-to-date on meningococcal or pneumococcal vaccines is the leading preventable risk factor.
- Group living: Dorms, millitary barracks.
- Medical history: Recent skull fractures, ear infections, or brain surgery.
- Pregnancy: Increases the risk of Listeria infection, which can cause meningitis in newborns.
Viral risk factors:
- Season: Viral cases often peak during the summer and early fall.
- Age: Children under age 5 are more susceptible to enteroviruses.
Diagnosis
Because meningitis can worsen quickly, testing focuses on confirming inflammation around the brain and spinal cord and identifying the cause.
Common Test
- Lumbar puncture (spinal tap): Collects spinal fluid to check for infection and inflammation. This is the primary test for meningitis.
- Blood tests: Help detect infection in the bloodstream and support diagnosis.
- CT scan: Sometimes performed before lumbar puncture to check for brain swelling or complications.
Results guide whether it's viral, bacterial, or another cause and determine urgent treatment.
Treatment
Treatment is entirely dependent on the cause. Bacterial meningitis is a medical emergency, while viral meningitis is often managed with supportive care.
Viral Meningitis
Most patients recover within 7 to 10 days. Treatment usually focuses on:
- Rest, hydration, and over-the-counter medications for fever and pain.
- Antivirals: If a specific virus like Herpes is suspected, doctors may use Acyclovir. Side effects can include nausea, headache, or changes in kidney function.
Bacterial Meningitis
This requires immediate hospitalization and IV antibiotics. Because the condition is so dangerous, doctors will often start "broad-spectrum" antibiotics before the test results even come back.
- Antibiotics: Ceftriaxone, Ampicillin, or Vancomycin. These are chosen based on the patient's age and the likely type of bacteria.
- Corticosteroids: Medications like Dexamethasone are often given alongside the first dose of antibiotics. This helps reduce the swelling around the brain, which can prevent hearing loss and neurological damage.
Prevention
Vaccination is the single most effective way to prevent the most devastating forms of meningitis.
Bacterial vaccines: Meningococcal vaccine, Pneumococcal vaccine, Hib vaccine
Viral prevention: Routine Immunizations for Influenza (Flu), Chickenpox (Varicella), and Shingles help prevent the primary infections that can occasionally lead to viral meningitis.