- POTS (Postural Orthostatic Tachycardia Syndrome) is a condition where the heart rate rises rapidly (by 30+ bpm in adults) when standing up.
- Common symptoms include dizziness, rapid heartbeat, fatigue, brain fog, and sometimes fainting.
- The condition affects blood flow regulation and is linked to nervous system dysfunction, low blood volume, or excess adrenaline.
- It most commonly affects women aged 15–50 and may be triggered by illness, surgery, trauma, or pregnancy.
- Diagnosis often involves a tilt table test and ruling out other causes like orthostatic hypotension.
- Treatment includes increased fluids and salt, compression garments, exercise, and medications to manage symptoms.
Overview
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that disrupts how your body handles gravity. It is a form of orthostatic intolerance, meaning symptoms appear when upright and usually ease when lying down. Your heart rate rises by at least 30 beats per minute when you stand up. This sudden surge can leave you dizzy, faint, or feeling like your body is out of sync.
The condition affects the autonomic nervous system, which normally keeps your heart rate and blood pressure stable during position changes.
Normally, when you stand up, your body’s autonomic nervous system quickly tightens blood vessels and slightly increases your heart rate to keep blood flowing steadily to your brain and organs. Most people barely notice this change, and symptoms like dizziness are rare and brief.
In POTS, that system malfunctions. Blood pools in the lower body, and the heart overcompensates to keep blood flowing to the brain.
Symptoms
POTS can cause a wide range of symptoms, most of which get worse when standing. The hallmark sign is a rapid increase in heart rate, more than 30 beats per minute in adults (or over 40 in teens) within 10 minutes of standing.
This sudden spike can lead to:
- Lightheadedness
- Dizziness
- Fainting or near-fainting
But the effects go beyond just heart rate. Many people feel weak or shaky, especially in their legs after standing for too long. Some describe a “rushing” sensation or a racing heart without any clear reason.
You might also notice palpitation, sweating or anxiety.
Non-Cardiac Symptoms
POTS also affects other systems in the body. These symptoms may include:
- Fatigue that doesn’t improve with rest
- Brain fog—trouble focusing, thinking clearly, or remembering
- Blurred or tunnel vision
- Chest discomfort or pressure
- Shortness of breath, especially during activity
- Sleep disturbances
Symptoms often flare up after activities like standing in the shower, walking through a store, or being in a hot environment. Even simple tasks can be exhausting.
POTS symptoms can come and go. Some people experience long stretches of improvement, followed by sudden relapses. This relapsing-remitting pattern is common and can make the condition feel unpredictable.
Prevalence
POTS affects an estimated 1 to 3 million people in the U.S., though the real number may be higher due to frequent misdiagnosis.
It primarily affects women between the ages of 15 and 50, but anyone can develop it. Many patients trace the onset of symptoms to a specific trigger, like a viral infection, injury, or major life event. Others notice symptoms gradually, without a clear cause.
In recent years, POTS has gained more attention due to its link with long COVID, especially in younger adults.
Because symptoms vary and don’t always follow a textbook pattern, it’s common for patients to see multiple doctors before receiving an accurate diagnosis.
Causes
The exact cause of POTS isn’t fully understood, but researchers believe it can result from several different underlying problems in the body’s autonomic nervous system.
- Neuropathic POTS: In this type, the small nerve fibers in the lower body don’t work properly. These nerves normally help blood vessels tighten when you stand. When they don’t, blood pools in the legs, and the heart races to compensate.
- Hyperadrenergic POTS: This form involves an overactive “fight or flight” response. The body releases too much adrenaline, causing symptoms like shakiness, anxiety, and a rise in both heart rate and blood pressure when standing.
- Hypovolemic POTS: Here, the body has a lower-than-normal blood volume. With less blood to circulate, the heart works harder and beats faster to maintain blood flow.
- Secondary POTS: Sometimes, POTS develops as a result of another condition. It can follow a viral illness, surgery, trauma, or pregnancy. It’s also seen in people with autoimmune diseases or connective tissue disorders like Ehlers-Danlos syndrome.
Risk Factors
POTS most commonly affects women between the ages of 15 and 50, with many cases beginning during the teen years or early adulthood. For some, symptoms start around puberty. While men and children can develop POTS, it’s less common.
What Can Trigger It?
In many cases, symptoms begin after a major physical stressor, such as:
- A viral illness
- Surgery
- A serious injury
- Pregnancy
These events can disrupt the autonomic nervous system, setting off the symptoms of POTS. For others, the condition develops gradually, without a clear starting point.
Other Risk Factors
- Family history: POTS sometimes runs in families, suggesting a possible genetic link, though no single gene has been identified.
- Autoimmune conditions: Disorders like lupus, Sjögren’s syndrome, and celiac disease are more common in people with POTS.
- Connective tissue disorders: Conditions such as Ehlers-Danlos syndrome (hEDS) are strongly associated with POTS.
- Chronic illnesses: Diabetes, sarcoidosis, and chronic fatigue syndrome (ME/CFS) have also been linked.
- Environmental factors: Long-term effects from chemotherapy, toxin exposure, or heavy alcohol use may increase risk.
POTS can also be part of long COVID, especially in younger adults, adding to the number of new cases in recent years.
Because symptoms vary widely and can mimic other conditions, many people go undiagnosed or are misdiagnosed for years.
Diagnosis
Diagnosing POTS can take time. That’s because its symptoms like dizziness, fatigue, and rapid heartbeat, overlap with many other conditions, including anxiety, chronic fatigue syndrome, and low blood pressure.
The process usually begins with a detailed review of your symptoms and medical history. Your doctor will likely check your heart rate and blood pressure while you're lying down and again after standing.
If your heart rate increases by 30 beats per minute or more in adults (or 40 bpm in teens) within 10 minutes of standing,without a significant drop in blood pressure, POTS may be suspected.
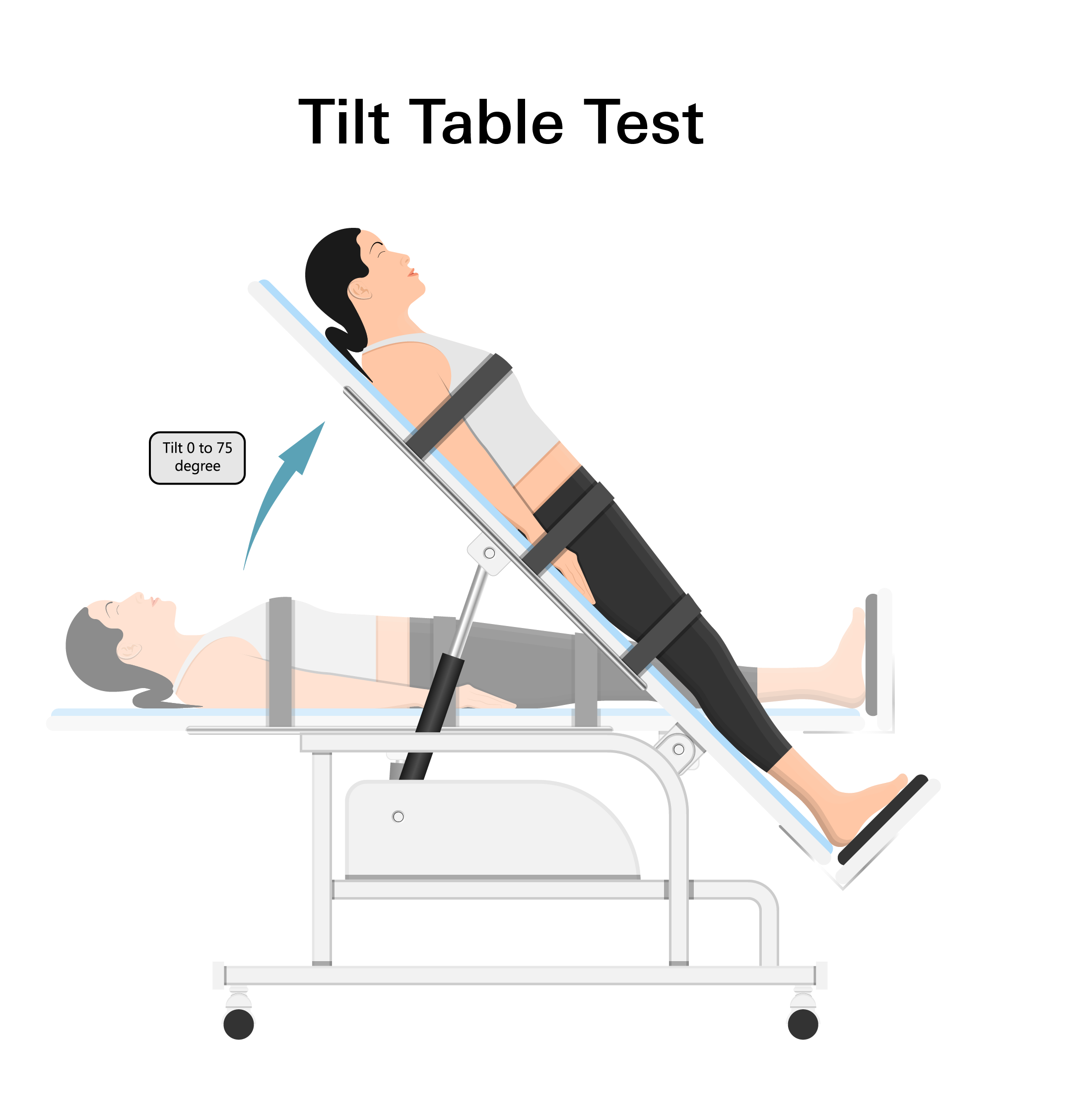
The most common test to confirm POTS is the tilt table test.
- You’re strapped to a table that tilts from lying flat to upright.
- Your heart rate, blood pressure, and sometimes oxygen or carbon dioxide levels are monitored.
- A diagnosis is likely if your heart rate jumps significantly, symptoms worsen while upright, and blood pressure stays relatively stable in the first 3 minutes.
Doctors will also rule out other conditions, like orthostatic hypotension, where blood pressure drops sharply upon standing. If that’s present, it’s not considered POTS.
In more complex cases, additional tests may be used:
- Valsalva maneuver: Measures how your nervous system responds to pressure changes.
- QSART: Tests how well your nerves control sweating.
- MRI or other scans: Used to rule out structural or neurological causes.
Treatment
There’s no one-size-fits-all treatment for POTS, but many people find relief through a combination of strategies:
Lifestyle Changes
- Increase salt and fluid intake to boost blood volume.
- Drink 16 ounces of water before getting out of bed to help with morning symptoms.
- Stay hydrated throughout the day.
Physical Activity
- Start slow and build up gradually.
- Exercise can improve circulation and reduce symptoms over time.
Compression Garments
- Wearing compression socks or abdominal binders helps prevent blood from pooling in the legs.
- This can reduce dizziness and improve energy levels.
Medications
Depending on your symptoms, your doctor may recommend:
- Fludrocortisone: Helps retain sodium and increase blood volume.
- Midodrine: Tightens blood vessels to improve blood flow when standing.
- Beta-blockers: Slow the heart rate and may help with tremors, anxiety, and brain fog.
Not every medication works for every person. It may take time to find the right combination, but many patients see meaningful improvements with the right plan.
Prevention
While POTS can’t always be prevented, there are ways to reduce symptom flare-ups and make daily life more manageable.
Stay Hydrated and Increase Salt Intake
- Drink plenty of fluids throughout the day to support blood volume and circulation.
- Many patients benefit from drinking water before getting out of bed, especially in the morning.
- Salty snacks or electrolyte drinks can help maintain fluid balance and reduce dizziness.
Helpful Daily Habits
- Avoid extreme heat and prolonged standing, which can worsen symptoms.
- Change positions slowly, don’t jump from lying down to standing.
- Plan breaks during the day to prevent fatigue and sudden energy crashes.
Exercise
- Light physical activity, introduced slowly, can improve tolerance to standing.
- Many patients start with seated or reclined exercises and gradually work up to more upright movement.
- Working with a physical therapist can help create a safe, personalized plan.
Use Compression Garments
- Compression socks or abdominal binders can help improve circulation and reduce blood pooling in the legs.
- These garments are especially helpful during long periods of standing or activity.
Be Proactive After Stressful Events
- Pay attention to how your body responds after illness, surgery, pregnancy, or injury.
- Recognizing early signs of POTS can lead to quicker management and better outcomes.
