Empowering Your Heart Health: The Value of Beta Blockers
- Beta blockers are mainly used to treat cardiovascular problems.
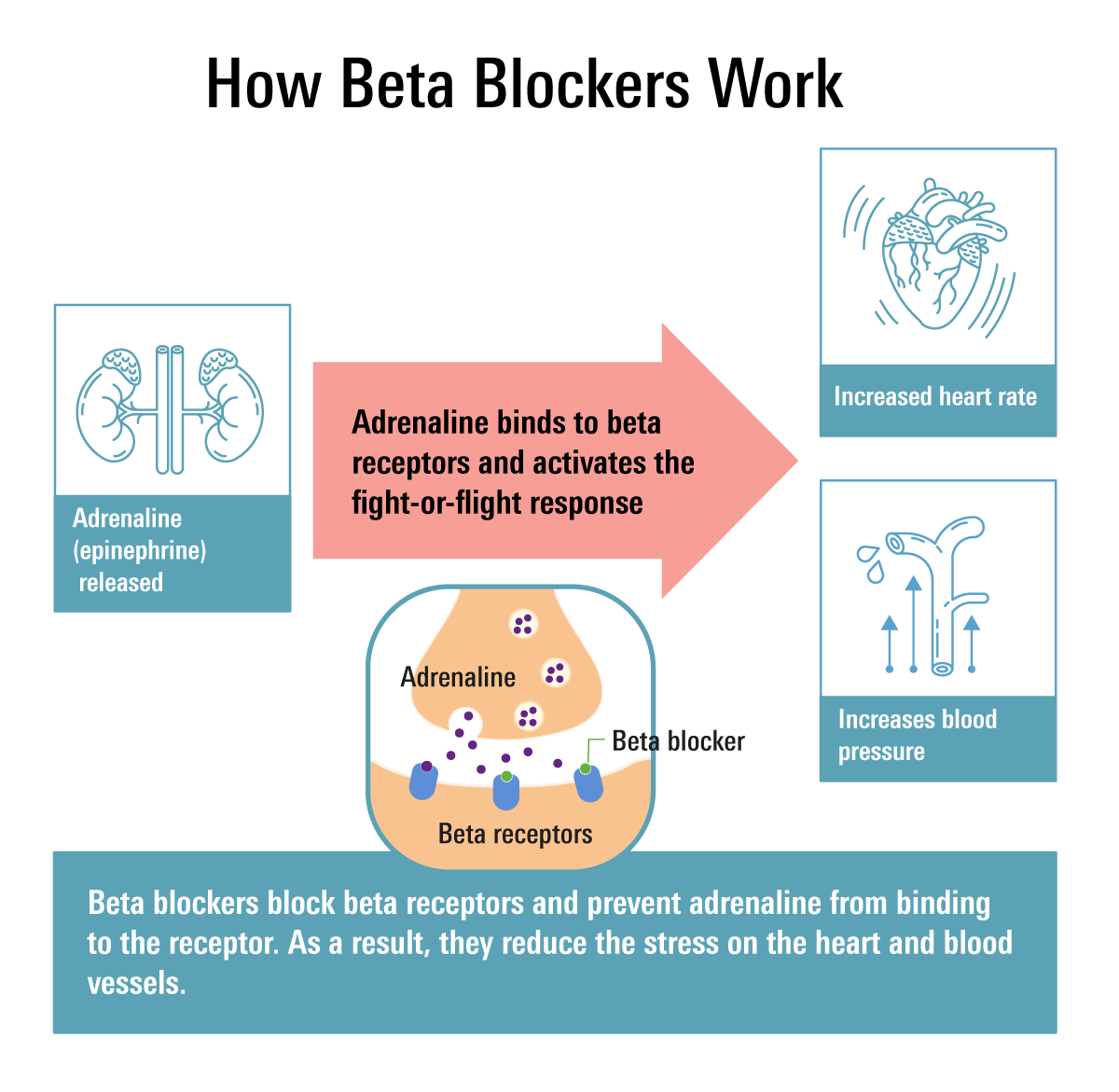
- They work by blocking beta receptors, so adrenaline can’t bind to beta receptors to activate the fight or flight response in your body.
- There are selective and non-selective beta blockers.
Selective beta blockers: atenolol, acebutolol, betaxolol, bisoprolol, metoprolol, bystolic
Non-selective beta blockers: nadolol, pindolol, propranolol, timolol, carvedilol, labetalol
Beta-blockers have been around since the 1960s, but there are now a variety of beta-blockers on the market, with many of them being used to treat various conditions. If you struggle with arrhythmia (irregular heartbeat), angina (chest pain), heart failure, and/or tremors, then beta-blockers may be a suitable drug class for you.
What are Beta-Blockers?
Beta-blockers, also referred to as beta-adrenergic blocking agents, are a drug class of medications, generally ending in “-olol,” used to prevent your heart from being affected by epinephrine (adrenaline), and other stress hormones such as noradrenaline.
Your body uses adrenaline and noradrenaline to activate your “fight-or-flight” response, which is designed to keep you safe during threatening scenarios. You may experience rapid heartbeat, high blood pressure, excessive sweating, anxiety, and heart palpitations if your body produces high adrenaline levels.
By hindering the release of these hormones, beta-blockers reduce the stress placed on your heart and the force of heart muscle contractions. As a result, the blood vessels in your heart, brain, and the rest of your body are relieved of that pressure.
How do Beta-Blockers Work?
Nerves across your body, as well as your adrenal gland (a small gland that produces steroid hormones), create norepinephrine and epinephrine. These hormones help control heart rate, blood pressure, and other important body functions. They work as neurotransmitters, which are chemicals used by nerves to communicate with one another. Your body has both alpha and beta receptors.
Beta-blockers differ by which receptors are blocked. Examples of beta receptors include:
- Beta-1 (β1)-adrenergic receptors
— Located in your eyes, heart, and kidneys - Beta-2 (β2)-adrenergic receptors
— Mainly located in your gastrointestinal tract (GIT), uterus, lungs, liver, blood vessels, and skeletal muscle - Beta-3 (β3)-adrenergic receptors
— Located in fat cells
Beta-blockers decrease your blood pressure by competitively blocking beta-1 and/or beta-2 adrenergic receptors, resulting in decreases in heart rate and cardiac muscle contractility.
Some medications in this drug class have alpha-1 blocking properties, such as Carvedilol and Labetalol, that decrease peripheral vasoconstriction, which is another mechanism used to lower your blood pressure.
Beta-blockers block the effects of catecholamines (a neurohormone that’s made by nerve cells and used to send signals to other cells), especially norepinephrine, at the beta-1 and beta-2 adrenergic receptors. This results in vasodilation (widening of blood vessels), improving your cardiac function, and improving your medical condition. For this reason, beta-blockers are recommended for all individuals with heart failure.
What are Beta-Blockers Used For?
Beta-blockers are primarily used to treat cardiovascular problems. These medications were previously used for hypertension (high blood pressure) treatment, however, are no longer recommended as a first-line treatment option for uncontrolled hypertension unless an individual has a comorbid condition for which beta-blockers are recommended, such as a previous heart attack, stable ischemic heart disease (SIHD), and/or heart failure, or if other medications, such as diuretics, haven't worked well.
Beta-blockers are commonly used to treat and/or prevent:
- Congestive heart failure — a cardiac condition that causes an accumulation of fluid in the lungs and other bodily tissues
- Angina — beta-blockers can prevent chest pains
- Hypertension — beta-blockers can decrease your blood pressure if it’s too high
- Arrhythmias — beta-blockers can control abnormal heart rhythms (irregular heartbeat)
- Myocardial infarction — beta-blockers can decrease the risk of a further heart attack if you have already experienced one
- Coronary heart disease — beta-blockers can lower your heart rate and blood pressure and reduce the workload on your heart
Beta-blockers are also used as off-label (used for a medical condition that it is not approved to treat) medications in these conditions:
- Glaucoma
— A medical condition where fluid builds up inside your eye, causing pressure to increase.
— Glaucoma is a prevalent cause of eyesight loss in older individuals.
— Eye drops containing beta-blockers, such as Timoptic ophthalmic solution, are frequently prescribed to lessen the production of fluid and pressure within the eye. - Migraines
— Propranolol and metoprolol are recommended as first-line treatment options for migraine prevention by the American Academy of Neurology and the American Headache Society.
— These beta-blockers can reduce the number of migraine attacks if the attacks occur frequently. - Anxiety
— Your stress hormones are blocked by beta-blockers, leading to relief of physical anxiety symptoms (i.e. trembling and sweating). - Essential tremors
— Hands, head, trunk, voice, or legs shake rhythmically due to a neurological disease called essential tremors (ET). — Propranolol and primidone are beta-blockers that can help in essential tremor management. t) - Overactive thyroid
— In individuals with an overactive thyroid, beta-blockers can help with symptoms including tremors and a fast heart rate, by blocking the thyroid hormone in your bloodstream.
Selective vs Non-selective Beta-blockers
Beta-blockers are divided into two categories: Selective and Non-selective.
Beta-1 selective blockers
Specifically developed to block the β1 receptors, which are found in your heart. Selective beta-blockers are used to treat cardiac conditions since they exclusively activate the β1receptors, which are concentrated in your heart tissue.
These beta-blockers are generally safe to use if you have diabetes because their activity is more specific/selective. They aren't a common therapeutic option for anxiety.
Examples include:
- Atenolol (brand: Tenormin) 25–100 mg daily
- Acebutolol 200–800 mg daily
- Betaxolol 5–20 mg daily
- Bisoprolol 2.5–20 mg daily
- Metoprolol tartrate (Lopressor) 100–450 mg daily
—Taken with or immediately after food - Metoprolol succinate extended-release (Toprol XL) 25–100 mg daily
—Taken with or immediately after food
Beta-1 selective blocker with nitric oxide-dependent vasodilation (widening of your blood vessels)
- Nebivolol (Bystolic) 5–10 mg daily
Non-selective beta-1 and beta-2 blocker
Non-selective beta-blockers can be used to alleviate some physical effects of anxiety in addition to treating specific heart conditions. Non-selective beta-blockers are not considered safe to use if you have diabetes.
- Nadolol (Corgard) 40-320 mg daily
- Pindolol 5-30 mg BID (twice a day)
- Propranolol (Inderal LA, Inderal XL)
—Inderal LA (long-acting): 80–160 mg daily
—Inderal XL (extended-release): 80 mg daily
—May be used for migraines and essential tremors - Timolol (Timoptic ophthalmic solution (eye drops)) 10–30 mg BID
—Used to treat glaucoma (open-angle type) or other eye diseases, such as ocular hypertension
Non-selective beta-blocker and alpha-1 blockers
- Carvedilol (Coreg, Coreg CR)
—IR (immediate-release): 6.25–25 mg BID
—CR (controlled-release): 20–80 mg daily —Taken with food - Labetalol 100–1,200 mg BID
—Drug of choice in pregnancy
What are the Side Effects of Beta-Blockers?
Common adverse effects of these medications include:
- Decreased heart rate
- Fatigue
- Hypotension (low blood pressure)
- Dizziness
- Depression
- Decreased libido (decreased sexual desire)
- Cold hands and/or feet
- Weight gain (seen specifically with metoprolol and atenolol)
- Diarrhea
- Stomach cramps
- Nausea
- Vomiting
What Should I Look Out For When Taking a Beta-Blocker?
Beta-blockers have a black box warning (the strictest warnings for prescriptions) that warns against abruptly discontinuing your beta-blocker because that may increase your risk of a heart attack or other heart problems.
Beta-blockers should be gradually tapered off (gradually decrease the dose) over 1–2 weeks to avoid serious side effects, such as acute tachycardia (sudden onset of a rapid heartbeat), hypertension (high blood pressure), and/or ischemia (deficient blood supply to parts of your body).
Individuals with diabetes should use beta-blockers with caution because they have been shown to potentially worsen hypoglycemia (low blood sugar) and hyperglycemia (high blood glucose) and mask hypoglycemia symptoms such as rapid heartbeat.
Individuals with bronchospastic disease, such as asthma or chronic obstructive pulmonary disease (COPD), should use beta-blockers with caution because they have been shown to trigger severe asthma attacks.
Speak With Your Doctor
For many illnesses, beta-blockers are the first-line treatment. Beta-blockers have especially helped many individuals with heart failure live a longer and healthier life.
Talk to your healthcare provider about using beta-blockers and send your prescription to Marley Drug. Save up to 95% compared to your local pharmacy by using Marley Drug