- Itchy eyes occur when irritants trigger histamine release, most commonly from seasonal/year-round allergies, dry eyes, contact lenses, or makeup.
- Symptoms include redness, watering, burning, grittiness, and urge to rub; see a doctor promptly for discharge, pain, swelling, or vision changes.
- Treatments range from OTC antihistamines and artificial tears to prescription steroids or mast cell stabilizers for severe cases.
- Prevention tips: avoid allergens, use preservative-free drops, follow the 20-20-20 rule, and keep eyes clean and hydrated.
Overview
Itchy eyes are one of the most frequent complaints eye doctors receive. The sensation generally indicates irritation on the surface of the eye or the tissues surrounding it.
How it works: The surface of your eyes and eyelids are lined with tiny nerve endings. When these nerves detect dryness or irritation, they signal the brain, which interpret as an itch. In response, the body releases histamine, a natural chemical that causes redness, tearing, and swelling. This process is biologically similar to an itchy mosquito bite, but it occurs in one of the most sensitive parts of the body.
How common is it?
Itchy eyes are very common, affecting millions of Americans annually.
Symptoms
Symptoms can range from a mild, ticklish sensation to severe discomfort that disrupts sleep and concentration.
Common sensations include:
- Strong urge to rub the eyes
- Redness or swollen eyelids
- Watery eyes
- Burning, stinging, or gritty feeling
- Mild light sensitivity
- Feeling that something is in the eye
Why you shouldn't rub your eyes: rubbing often makes the itching worse. Scratching the delicate surface releases more histamines, which intensifies the itch.
See your doctor promptly if you have::
- Thick, colored (yellow/green) discharge
- Pain or swelling around the eye
- Blurred vision that doesn’t clear with blinking
- Crusting of eyelids or lashes that keeps returning
- New sensitivity to light so strong you can’t open your eyes
- Severe light sensitivity
- Symptoms in only one eye that then spread (possible infection)
Go to urgent care or the nearest emergency room for sudden vision loss, severe pain, or significant swelling. These can be signs of a more serious problem.
Causes
Itchy eyes usually stem from a reaction to pollen, makeup, or underlying issues like dryness.
Common Causes:
- Allergic conjunctivitis: Overreaction to allergens such as pollen, pet dander, or dust releases histamine causing redness, tearing, and itch
- Dry eye syndrome: Insufficient tear production or quick tear evaporation makes the eyes dry, sore, and itchy. Screen time, dry air, and contact lenses can worsen this
- Everyday irritants: Smoke, wind, perfume, chlorine from pools, and dust can irritate eyes
- Medications: Some birth control pills, hormone treatments, antidepressants, and blood pressure medicines can cause dry or itchy eyes
- Contact lenses and solutions: Prolonged wear or reactions to cleaning solutions can cause irritation
- Eye infections: Conjunctivitis (pink eye) and other infections cause itching, redness, and discharge
- Eyelid inflammation (blepharitis): Oil gland blockage or skin flakes on eyelid edges cause itchiness and crusting
Risk Factors
You are at higher risk if you:
- Have hay fever or other allergies
- Spend many hours on screens or in dry/air-conditioned environments
- Wear contact lenses (especially extended-wear)
- Are over age 50 (tear production drops with age)
- Are female (hormonal changes affect tear film)
- Have autoimmune diseases (Sjögren’s, rheumatoid arthritis, lupus)
- Live in dry, windy, or high-pollen areas
- Take medications that reduce tear production
Having several risk factors together usually makes symptoms worse.
Diagnosis
If irritation persists, a diagnosis helps distinguish between allergies, infections, or dryness. You can visit an optometrist, ophthalmologist, or sometimes a primary care doctor.
What to expect during a visit:
- History review: Discussion of symptoms, symptom timing, and medication use
- Physical exam: The doctor will use a slit-lamp microscope to examine the eyelids, tear film, and eye surface
- Tear analysis: Checking tear amount and quality to rule out dry eye
- Allergy testing: Skin or blood tests may be used to identify specific allergens.
Treatment
Treatment depends on the underlying cause. Mild cases often respond to over-the-counter (OTC) remedies, while severe cases may require prescriptions.
OTC Options
Oral Antihistamines
Great when itchy eyes come with sneezing, runny nose, or full-body allergies. The newer (“second-generation”) ones almost never cause drowsiness.
| Zyrtec (Cetirizine 10 mg) | Adults & kids 6+: 10 mg once daily (5 mg for mild symptoms). Starts working fastest; many say it’s strongest |
| Claritin (Loratadine 10 mg) | Adults & kids 6+: 1 tablet daily |
| Allegra (Fexofenadine 180 mg) | Adults & kids 12+: 180 mg once daily. Good for outdoor allergies |
| Xyzal (Levocetirizine 5 mg) | Adults & kids 12-64: 5 mg once daily evening (or 2.5 mg for mild symptoms); Kids 6-11: 2.5 mg once daily evening. Slightly stronger than Zyrtec for some people |
Benadryl (diphenhydramine) works but makes most people sleepy and can dry eyes more. Only use occasionally or at night.
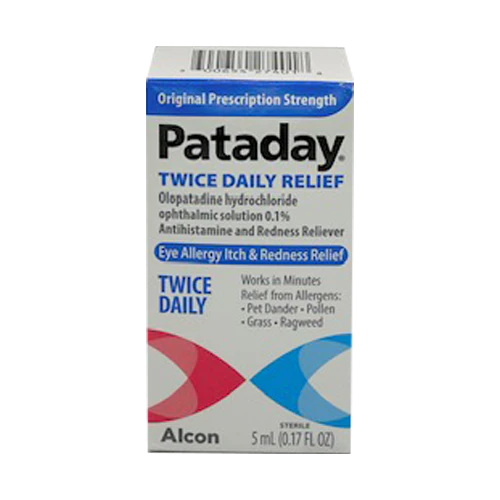
Allergy Eye Drops (Antihistamine + Mast-Cell Stabilizer)
These are the gold standard for itchy allergy eyes. They relieve itching fast AND prevent it from coming back. Eye doctors almost always recommend these first for seasonal or year-round eye allergies. Safe for long-term/seasonal use.
| Pataday Extra Strength (Olopatadine 0.7%) |
|
| Pataday Once Daily Relief (Olopatadine 0.2%) |
|
| Xyzal (Olopatadine 0.1%) |
|
| Lastacaft (Alcaftadine) |
|
| Zaditor (Ketotifen) |
|
Redness-Reliever Drops (Decongestant + Antihistamine)
These drops provide quick relief for redness and mild itching but DO NOT use longer than 3 days. They cause rebound redness (eyes get worse when you stop).
| Opcon-A, Naphcon-A, Visine-A (Naphazoline + pheniramine) |
|
| Clear Eyes Redness Relief (Naphazoline + glycerin: lubricant) |
|
Prescription Options
| Alomide (lodoxamide) |
|
| Alocril (nedocromil) |
|
| Loteprednol (Lotemax, Alrex) |
|
| Ketorolac (Acular) |
|
Prevention
You can't always stop itchy eyes from happening, but small, consistent changes make a big difference. The goal is to reduce irritants and keep the eye surface hydrated.
Allery Avoidance (Biggest Impact)
- Track pollen daily: Use a weather app or pollen.com. When high: stay inside peak hours (morning), keep windows closed, run AC, shower + change clothes after outdoors.
- HEPA air purifier in bedroom: Reduces indoor allergens up to 50–70%. Worth every penny if you have pets or carpet.
- Wash allergens off face/eyelids nightly: Baby shampoo on a washcloth or lid scrub or hypochlorous acid spray (Avenova, Heyedrate) — game changer for blepharitis-related itch.
Eye-Specific Habits
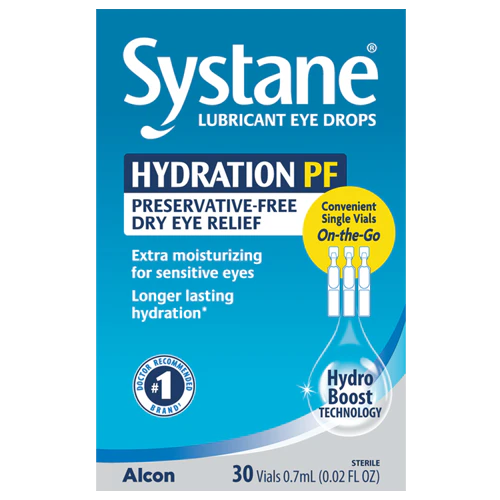
- Preservative-free artificial tears: Use anytime (Refrigerate for extra relief). Best if you use drops >4× day.
- 20-20-20 rule: Every 20 min, look 20 ft away for 20 seconds — prevents dryness itch from screens.
- Rinse your eyelids regularly: Gently clean along your lash line with a warm, damp cloth or a lid-cleansing wipe once a day. This removes oil, dust, and bacteria that can trigger inflammation or blepharitis.
- Wraparound polarized sunglasses: Blocks pollen, wind, UV. Huge difference outdoors.
- Stay hydrated and include omega-3 fats: Omega-3s from salmon, chia seeds, and flaxseed oil can improve tear quality and reduce dryness. Aim for a mix of hydration and healthy fats daily.
- No scented products near face: Hairspray, perfume, fabric softener — apply after makeup/contacts or in another room.
- Change contact lenses as directed: Over-wearing lenses or sleeping in them increases dryness and irritation. Try switching to daily disposable lenses if you have recurring symptoms.
Related Topics
Best Products for Treating Itchy Eyes
Itchy eyes are a common problem with many possible causes — from seasonal allergies and dryness to irritation from smoke, screens, or contact lenses. In some cases, infections or sensitivities can also play a role.