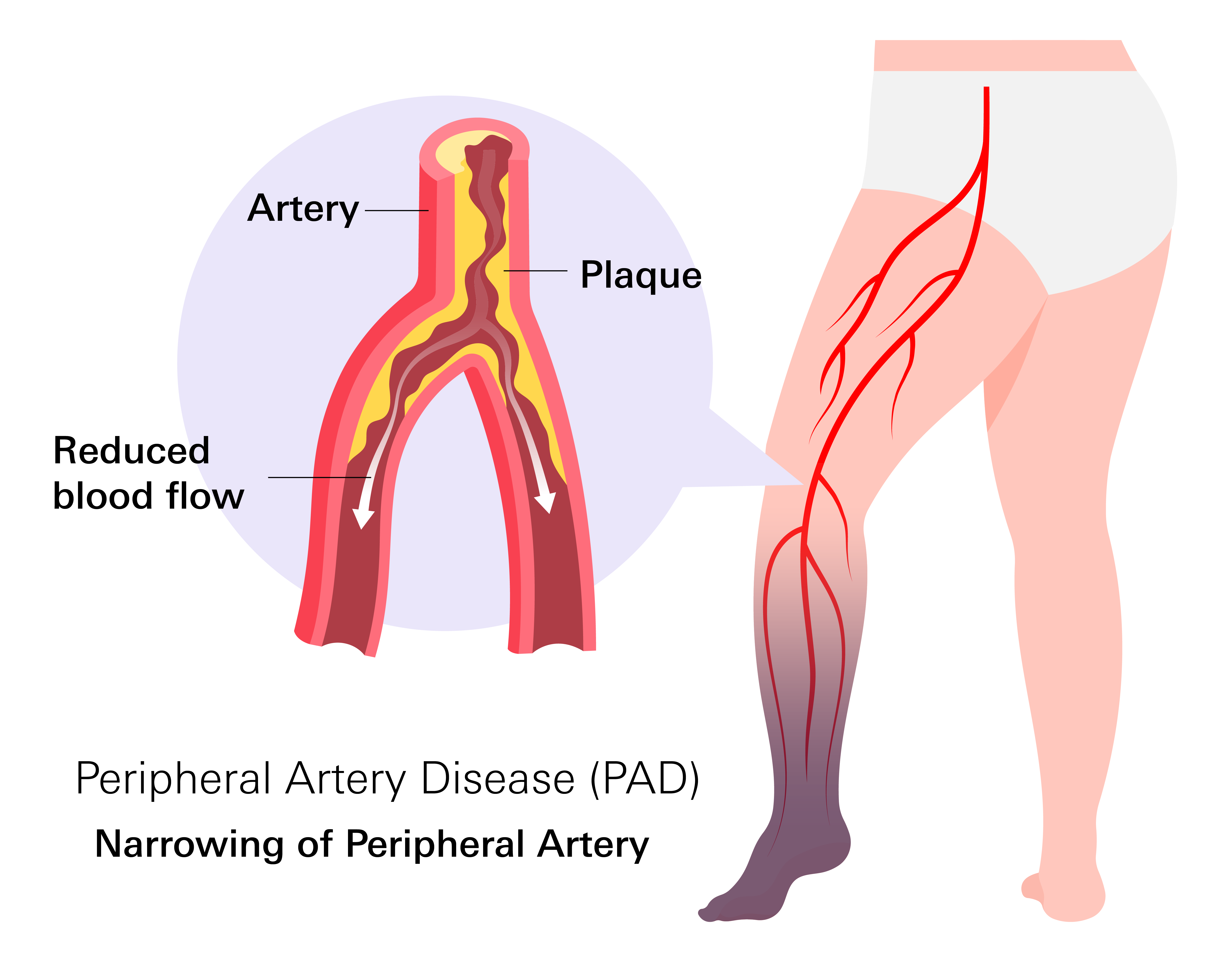
- Peripheral artery disease (PAD) is a condition where arteries in the legs and feet become narrowed, and reduce blood flow.
- Symptoms can vary depending on the extent of reduced blood flow. Common symptoms include leg pain during walking, leg weakness, cold or numb feet, slow-healing wounds, and changes in skin or nails. Serious symptoms requiring immediate medical attention include rest pain, discolored skin, non-healing ulcers, severe numbness, and sudden, intense leg pain.
- Risk factors include smoking, diabetes, high blood pressure, high cholesterol, older age, family history of heart disease or stroke, obesity, inactivity, and chronic kidney disease.
- PAD is a long-term condition, but it can be managed, and early identification is crucial to prevent worsening symptoms and complications.
- Treatment includes lifestyle changes, medications, supervised exercise therapy, and surgical procedures like angioplasty, stenting, bypass surgery, and atherectomy.
Overview
Peripheral artery disease (PAD) is a condition that affects the flow of blood in the arteries outside of your heart, most commonly in your legs and feet.
Arteries are blood vessels that carry oxygen-rich blood from your heart to the rest of your body. In PAD, these arteries become narrowed, making it difficult for enough blood to reach your legs and feet. This reduced blood flow can cause discomfort, slow-healing sores, and trouble walking.
The most common sign is pain or cramping while walking, which improves with rest. In more advanced cases, blood flow can become so limited that even minor injuries on your feet or toes take much longer to heal.
PAD is a long-term condition, but there are ways to manage it and improve blood circulation. Identifying this condition early can help prevent worsening symptoms and complications.
Prevalence
According to the Centers for Disease Control and Prevention (CDC), it's estimated that 6.5 million Americans over the age of 40 have PAD. However, the actual number may be even higher because many individuals do not experience symptoms or mistake them for normal signs of aging.
The likelihood of developing PAD increases with age. Research indicates that between 12% and 20% of adults over the age of 65 are affected by this condition.
Despite its prevalence, PAD is often underdiagnosed, especially in its early stages. Many people do not have noticeable symptoms, or they assume that leg pain during walking is just a part of getting older. This can lead to delays in diagnosis and treatment, which increases the risk of more serious health problems.
Stages and Symptoms
Doctors classify PAD into four stages based on how much it affects blood flow and daily activities:
Stage 1: Asymptomatic PAD (No Symptoms)
In the early stage, blood flow is reduced, but there are no noticeable symptoms. Your body may still get enough oxygen through smaller blood vessels that try to compensate for the narrowing arteries. Many patients are unaware they have PAD at this point unless a doctor finds it during a routine check-up or a test measuring blood circulation in the legs.
Stage 2: Claudication (Leg Pain During Exercise)
- Leg pain or cramping during walking or exercise that improves with rest.
- Weakness or fatigue in the legs after activity.
As PAD progresses, reduced blood flow starts to cause discomfort, especially during physical activity. The most common symptom is claudication, which is cramping, aching, or heaviness in your legs, usually in your calves, thighs, or buttocks. The pain happens when walking or exercising but improves with rest. This occurs because the muscles are not getting enough oxygen when working harder. Over time, even short walks may become uncomfortable.
Stage 3: Critical Limb Ischemia (Resting Pain and Wounds That Don’t Heal)
- Pain in the feet or toes even when resting.
- Pain that is often worse at night.
- Non-healing wounds or sores on the feet or toes.
- Coldness or numbness in the feet or toes.
- Changes in the skin of the feet and legs (shiny, thin, dry, or discolored).
At this stage, blood flow is severely restricted, causing pain even when at rest. The pain is often worse at night when lying down because gravity is no longer helping blood reach your feet. Some patients find relief by hanging their legs off the side of the bed or sleeping in a chair to improve circulation.
Since your legs and feet are not getting enough oxygen, wounds, cuts, or sores may take much longer to heal. In some cases, they may not heal at all. The skin on your feet and toes may appear shiny, dry, or discolored. If left untreated, this stage can lead to serious complications.
Stage 4: Acute Limb Ischemia (Severe Blockage and Tissue Damage)
- Sudden and severe pain in the leg or foot.
- Extreme coldness, numbness, or paleness of the affected limb.
- Darkened or black skin, indicating tissue death.
- Presence of non-healing ulcers or open wounds.
- Inability to move the foot or toes.
This is the most severe stage of PAD and requires immediate medical attention. Blood flow to the affected limb is almost completely blocked, leading to sudden and severe pain, coldness, numbness in the toes or feet, and the development of ulcers or tissue death (gangrene).
The skin may appear darkened or black in areas where tissue is dying. Without prompt treatment, acute limb ischemia can cause permanent damage, and in extreme cases, amputation of the affected limb may be necessary to prevent infection from spreading.
Causes
PAD happens when blood has trouble flowing through the arteries in your legs and feet because they become too narrow, blocked, or clogged.
- Atherosclerosis (Plaque buildup in the arterties): Most common cause. Plaque is made of fat, cholesterol, and other substances in your blood. Over time, it hardens and makes it difficult for blood to pass through.
- Blood blot: In some cases, blood clots can suddenly block an artery, cutting off blood flow.
- Inflammation and Injuries: Inflammation in the arteries, which can happen due to certain infections or immune system problems, may also cause narrowing. Injuries to the arteries from accidents or surgery can also lead to scarring that makes blood flow harder.
Risk Factors
Certain factors increase the chances of developing PAD, especially those that affect blood circulation and artery health. Some of these risks can be managed, while others cannot be changed.
Smoking
Smoking is one of the strongest risk factors for PAD. The chemicals in cigarettes damage the arteries, making them more likely to narrow and form blockages. Smoking also reduces oxygen levels in the blood, further affecting circulation. Even those who quit smoking remain at higher risk compared to those who never smoked.
Diabetes
Diabetes affects how the body processes sugar, but it also damages blood vessels over time. High blood sugar can make the arteries stiff and more prone to plaque buildup, increasing the risk of PAD. Those with diabetes are also more likely to develop severe PAD, leading to slow-healing wounds and infections in the legs and feet.
High Blood Pressure (Hypertension)
High blood pressure forces the arteries to work harder than normal. Over time, this can cause them to thicken, narrow, and become less flexible, reducing blood flow to the legs. The longer blood pressure stays high, the greater the risk of developing PAD.
High Cholesterol
Cholesterol is a fatty substance in the blood, and too much of it can lead to plaque buildup inside the arteries. LDL cholesterol, often called "bad cholesterol," contributes to the thickening and hardening of the arteries, making PAD more likely. Keeping cholesterol levels in a healthy range can help slow the progression of artery narrowing.
Age (50 and Older)
As you get older, the risk of PAD increases. The arteries naturally stiffen with age, and years of wear and tear make plaque buildup more common. PAD is most frequently diagnosed in adults over 50, but the chances are even higher in those over 65.
Family History of Heart Disease or Stroke
If close relatives have had heart disease, strokes, or PAD, the risk is higher. This is because genetic factors can affect how the body processes cholesterol, blood sugar, and inflammation, all of which contribute to artery narrowing.
Obesity and Inactivity
Carrying extra weight puts more strain on the heart and blood vessels, increasing the risk of high blood pressure, diabetes, and high cholesterol—all of which contribute to PAD. A lack of movement can also make circulation worse, leading to weaker blood vessels and reduced oxygen supply to the legs.
Chronic Kidney Disease
Kidney disease affects how the body removes waste and regulates blood pressure. It is linked to higher rates of inflammation and artery damage, making PAD more likely.
Diagnosis
If you have symptoms that suggest Peripheral Arterial Disease (PAD), your doctor can perform tests to check how well blood is flowing in your legs. Since PAD develops gradually, it may not always be obvious at first, but several tests can help confirm the diagnosis.
- Ankle-Brachial Index (ABI): This is a quick, painless test that compares the blood pressure in your ankle to the blood pressure in your arm. If the pressure in your ankle is much lower than in your arm, it may mean that blood is not flowing well to your legs. This test helps detect PAD early and is often the first step in diagnosis.
- Ultrasound: An ultrasound uses sound waves to create images of your blood vessels and can show whether a blockage or narrowing is affecting circulation. A specific type, called Doppler ultrasound, measures how fast blood is moving through the arteries, helping doctors see if blood flow is restricted.
- Angiography: This procedure uses a contrast dye injected into your bloodstream to make the arteries visible on an X-ray. This test helps identify the exact location and severity of a blockage. It is usually done when a doctor is considering treatment options such as placing a stent or performing surgery.
- CT Angiography: This test uses X-rays and a contrast dye to show clear images of blocked or narrowed arteries.
- Magnetic Resonance Angiography (MRA): This test uses magnets and radio waves instead of radiation, making it a good option for those who should avoid X-rays.
Treatment
PAD treatment focuses on improving blood flow to your legs and lowering your risk of complications. Depending on the severity, managing PAD may involve lifestyle adjustments, medications, or medical procedures. For many patients, early treatment can help reduce symptoms and improve mobility.
Lifestyle Changes to Support Circulation
- Quitting Smoking: Smoking damages arteries and worsens PAD. Stopping can help slow disease progression and improve blood circulation.
- Healthy Eating: A diet high in fiber and low in saturated fat, cholesterol, and sodium can help manage risk factors such as high cholesterol and high blood pressure. Reducing unhealthy fats and avoiding trans fats found in processed foods can help prevent further artery narrowing.
- Managing Other Health Conditions: Keeping conditions such as diabetes, high blood pressure, and high cholesterol under control can help protect artery health.
- Taking Care of Your Feet and Skin: Since PAD reduces circulation, wounds on the feet may heal more slowly. Keeping the skin moisturized, trimming nails carefully, and checking for cuts or sores regularly can help prevent infections.
Exercise Therapy
Exercise therapy is often recommended for patients who experience pain while walking. A supervised program typically involves walking on a treadmill at least three times per week under medical guidance. This type of structured exercise has been shown to increase walking endurance and reduce leg discomfort.
Patients are also encouraged to continue walking at home for at least 30 to 60 minutes daily. The Start/Stop method—walking until discomfort appears, resting until it goes away, and repeating the process—can help build endurance and improve circulation over time.
Medications
- Antiplatelets: These help prevent blood clots from forming inside narrowed arteries. Common options include aspirin and clopidogrel (Plavix).
- Cholesterol-Lowering Medications: Statins, such as atorvastatin (Lipitor), rosuvastatin (Crestor), and simvastatin (Zocor), lower cholesterol levels and slow the buildup of plaque inside the arteries.
- Blood Pressure Medications: Medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) may be prescribed to help keep blood pressure in a healthy range.
- Cilostazol (Pletal): This medication helps expand blood vessels and improve circulation in your legs.
- Anticoagulants: In some cases, blood thinners such as rivaroxaban (Xarelto) may be recommended to reduce your risk of clotting.
Surgical Procedures
For some patients, lifestyle changes and medications may not be enough to relieve symptoms, especially if blood flow is severely restricted. In these cases, medical procedures may be needed to open the arteries and restore circulation. Some procedures include:
- Angioplasty: A small balloon is inserted into the narrowed artery and inflated to push plaque against the artery walls in order to improve blood flow.
- Stents: Often placed during angioplasty, stents are tiny metal mesh tubes that help keep the artery open and prevent it from narrowing again.
- Peripheral Artery Bypass Surgery: If an artery is severely blocked, a surgeon may create a new pathway for blood to flow by using a healthy blood vessel from another part of your body or a synthetic graft.
- Atherectomy: This procedure removes plaque buildup from inside the artery using a small cutting device or laser, helping to restore better blood flow.
Related Topics
Cholesterol: What It Is and Why You Should Care
Cholesterol is a waxy substance found in your blood that comes from either your liver or from the foods you eat such as meat, dairy and processed foods. Not all cholesterol is bad; your body uses some of it to help make cells, hormones and vitamins, but it is possible to have too much.
Blood Thinners Don’t Really “Thin” Blood
Blood thinners, also known as anticoagulants, are medications that help prevent the formation of blood clots. They are commonly used to treat conditions involving the risk of blood clots, such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and certain heart conditions.
Which DOAC Is Best for You
DOACs are a newer type of blood thinners that prevent blood clots and treat conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as to prevent stroke in people with atrial fibrillation.
Why is it important to manage your blood pressure?
If blood pressure is elevated for too long it puts strain on the body and can lead to several serious and permanent health complications and conditions

