- High cholesterol occurs when fatty deposits accumulate within blood vessels, a situation often caused by excessive levels of Low-Density Lipoprotein (LDL).
- High cholesterol is known as the ‘silent killer,’ as it seldom presents noticeable symptoms. Many individuals remain unaware of their high cholesterol levels until they suffer a significant cardiovascular event, such as a heart attack or stroke.
- Given its asymptomatic nature, the only reliable method to detect high cholesterol is through a blood test.
- When diet and exercise are not enough, statins are prescribed. Statins work by blocking an enzyme in our livers which produce.
- There are 7 statins on the market and pravastatin and pitavastatin have a reduced potential for drug to drug interactions when you are on multiple medications.
Overview
Cholesterol is an important building block that our body uses to build cells, and to make hormones, vitamin D, and bile salts which our bodies require everyday. Cholesterol is found in our blood and comes from 2 primary sources.
- Produced by our livers
Cholesterol synthesis occurs by enzymes in our liver and accounts for around 80% of our total cholesterol in our blood. - From our Diet
Cholesterol is absorbed by the intestines, from the food you eat.

LDL vs HDL
There are two main types of cholesterol;
- Good cholesterol: high-density lipoprotein, or HDL-C—helps to get rid of LDL by picking it up and taking it to your liver so your body can remove it from your body
- Bad cholesterol: low-density lipoprotein, or LDL-C—too much of this can be a problem as it can build up in your arteries.
If untreated high cholesterol can lead to the accumulation of plaque in our arteries increasing ones risk of having a heart attack or stroke.
High Cholesterol
High cholesterol occurs when fatty deposits accumulate within blood vessels, a situation often caused by excessive levels of cholesterol, particularly Low-Density Lipoprotein (LDL).
Over time, this condition can lead to the formation of plaque—a buildup of fats, cholesterol, and other substances in the arteries. This condition is called atherosclerosis. Plaque buildup narrows and can eventually block the arteries, restricting blood flow. When a large plaque ruptures or severely narrows an artery, it can cause a heart attack or stroke.
High cholesterol is known as the ‘silent killer,’ as it seldom presents noticeable symptoms. Many individuals remain unaware of their high cholesterol levels until they suffer a significant cardiovascular event, such as a heart attack or stroke. These events are often the culmination of years, sometimes decades, of untreated high cholesterol.
Causes
Some of the causes of high cholesterol are in our control, whereas others are not.
Cholesterol levels go up as we age. The bad cholesterol (LDL-C) rises after the age of 20 and reaches a plateau between age 60 to 70. This rise is more rapid in men than in women, however, after menopause, it tends to rise in women more rapidly.
Genetics can also play an important role in the levels of cholesterol in your blood. This is why your healthcare provider will ask you about your family history. If you have a close relative who has high cholesterol, your risk is higher. People of certain ethnicities are also more likely to have high cholesterol then others.
For most, a poor diet and lack of exercise are the two main causes of high cholesterol. Approximately 75% of the cholesterol in our blood is produced by our liver. The remaining 25% comes from our diet.
Risk Factors
- Diet heavy in trans and saturated fats
- Sedentary lifestyle
- Overweight or obese
- Excessive alcohol consumption
- Smoking
- Diabetes
- Age
- Gender
- Genetics: Familial Hypercholesterolemia
Diagnosis
Given its asymptomatic nature, the only reliable method to detect high cholesterol is through a blood test. Regular screening is essential for early identification and management of high cholesterol, aiming to prevent cardiovascular diseases.
Some markers which your healthcare provider will test for include:
- Low Density Lipoprotein (LDL) Cholesterol.
Normal: less than 100 mg/dL - High Density Lipoprotein (HDL) Cholesterol.
Normal range: Higher than 40 mg/dL for men. Higher 50 mg/dL for women - Triglycerides: A fat that is linked to heart disease.
Normal: below 150 mg/dL - Apolipoprotein B: A high-risk marker and predictor of cardiovascular disease
- Total Blood Cholesterol: Defined as your HDL + LDL + 20% Triglycerides.
Normal: less than 200 mg/dL
Read more on What Do Your Cholesterol Test Results Mean?
Lifestyle
Diet and exercise are the first thing your healthcare provider will ask you to change if you are diagnosed with high cholesterol.
Here are 6 things you can do to help lower your cholesterol levels:
- Decreasing stress
- Exercising at least 3 times a week for 30 minutes
- Maintaining a healthy weight
- Improve your diet by incorporating more fruits and vegetables into your diet and less saturated or trans fats
- Avoid excessive alcohol consumption
- Avoid smoking
Statin Therapy
Statins are the first line of defense to lower your cholesterol. When diet and exercise are not enough, statins are the first line of defense when it comes to lowering cholesterol. Statins work by blocking an enzyme in our livers which produce cholesterol, reducing our bodies overall cholesterol levels.
40–75% Will Stop Taking Their Statin In The First Year
Muscle pain is one of the more common side-effects from statin therapy. 62% of former statin users indicated that side-effects was the reason they stopped taking their medication.
Newer statins, like pitavastatin, are now available in the U.S and may be good options for those who have stopped taking their statin. In clinical studies, rate of muscle pain are only 3.1% with pitavastatin.
Don't Give Up On Your Statin. Not all Statins are the Same. There are 7 different statins. While they all lower cholesterol, there are some key differences to consider.
The current statins available in the U.S. include atorvastatin (Lipitor), fluvastatin (Lescol XL), lovastatin (Altoprev), pravastatin (Pravachol), rosuvastatin (Crestor), simvastatin (Zocor), and most recently approved pitavastatin (Zypitamag, Livalo).
Read about Statin Intolerance
What to Consider When Choosing a Statin
Are you taking other medications?
Most statins are metabolized by an enzyme called cytochrome P450 (CYP450). Unfortunately, 70-80% of medications are also processed by the same family of enzymes. When these enzyme pathways become too busy it can lead to drug interactions.
There are only two statins which have very limited interactions with this pathway, pitavastatin, and pravastatin. Because of this key difference, they both have a reduced potential for interactions many commonly prescribed medications.
Are you diabetic, or prediabetic?
Increases in blood sugar levels have been seen with statin medications. While all statins do have a warning and precaution that they can raise HbA1c and fasting serum glucose levels, there is data to suggest that this may not be the same across all statins.
For example, a clinical study compared pitavastatin (4 mg) with atorvastatin (20 mg) in those living with Type 2 Diabetes. They found that while cholesterol lowering effects of the medications were similar, only the atorvastatin group saw a significant increase in blood glucose levels.
If you have Type 2 Diabetes, or are worried about your glucose levels, ask your healthcare provider about pitavastatin.
Are you currently experience statin side effects?
While statins are generally well-tolerated, they are not without their risk of side effects. The most common side effect is muscle pain, and this goes up with dose of statin.
If you are currently having issues with your statin be sure to talk to your healthcare provider.
Newer statins like pitavastatin have rate of muscle pain of 3.1% and may be a good statin option for you.
Do you drink grapefruit juice?
Some statins interact with grapefruit juice and this can lead to statin side effects.
In fact, grapefruit juice is well-known to have an effect on several medications. Grapefruit juice interacts with the same enzyme our bodies use to break down atorvastatin (Lipitor), simvastatin (Zocor), and lovastatin (Altoprev).
If you enjoy grapefruit juice, you should consider statins like rosuvastatin (Crestor), pravastatin (Pravachol) and pitavastatin (Zypitamag).
Are you of Asian descent?
Certain statins, like rosuvastatin (Crestor) have dose restrictions for people of Asian descent. Newer statins, like pitavastatin (Zypitamag), do not have this same dose limitation.
Are you taking any antiretroviral therapy?
Most statins including atorvastatin (Lipitor), rosuvastatin (Crestor), simvastatin (Zocor), fluvastatin (Lescol XL), and lovastatin (Altoprev) can interact with certain antiretroviral medications.
Statins like pravastatin (Pravachol) and pitavastatin (Zypitamag) do not appear to have this same limitation. If you're taking antiretroviral therapy be sure to tell your healthcare provider.
Have you reached your cholesterol lowering goals?
If you haven't reached your cholesterol lowering goals you may need to make some additional changes. You have many options. You can increase the dose of your statin which should add an additional ~6% decrease in your bad cholesterol. You can also add on additional therapies such as ezetimibe to your statin regimen.
Another important thing to consider is your lifestyle. If you're not at your target yet, you may want to consider making additional changes to the foods you eat and the amount of exercise you are doing.
Most importantly, talk with your healthcare provider to come up with a plan to achieve your cholesterol goals.
Combination Therapy
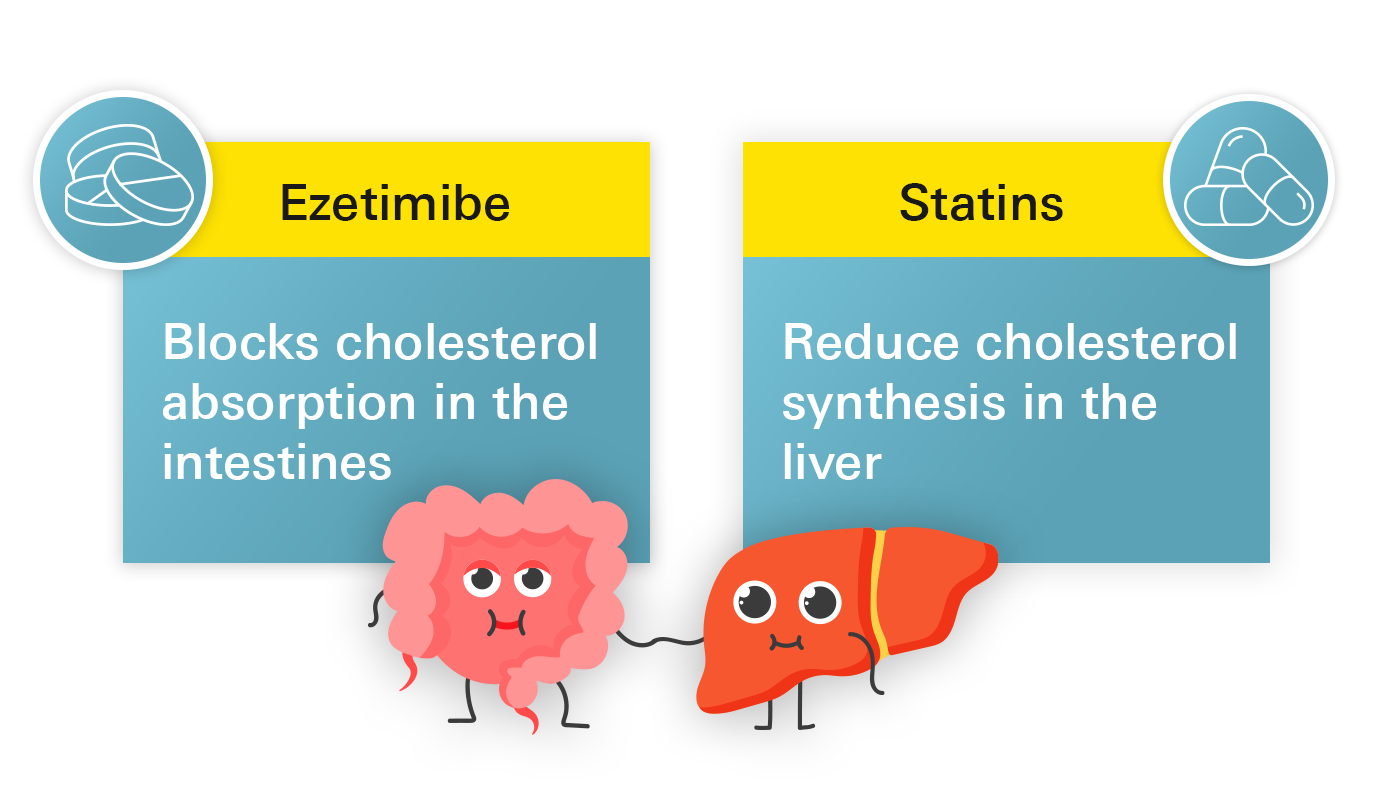
If you are unable to achieve the desired level of LDL-C reduction with a statin, your healthcare provider may increase the dose of your statin, or suggest additional therapies, also known as combination therapy.
The most common add-on combination therapy is ezetimibe (generic Zetia®). Until recently when ezetimibe's patent life ended it was extremely expensive. But now, with increased competition of generic manufacturers we have been able to add ezetimibe to Marley Drug's Wholesale List.
Cholesterol and Inflammation
When cholesterol deposits buildup inside your blood vessels, your immune system may recognize this substance as a foreign invader and sends white blood cells to gobble it up. This creates plaque. These plaques grow over time as more cholesterol is deposited on your blood vessels and more white blood cells are sent to help.
During chronic inflammation, these white blood cells deposited in these plaques can become overactive and this can contribute to plaques becomes unstable.
As you can imagine, blood is constantly flowing by these plaques. If they are unstable this increases the likelihood one of them may break off. When they break off this can be very dangerous. Either the plaque can get lodged further down stream and cause a blockage in a smaller blood vessel, or your body may recognize the ‘breakoff’ site as an injury and respond to it.
To explain how this works, think of a cut. Your bodies goal is to stop the bleeding, so it sends a certain cell in your blood called platelets, whose job is to create a barrier and stop the bleeding. Your body also recognizes a ruptured plaque in your blood vessel as a cut. It doesn’t know the difference. So it does the same thing it would with a cut, it sends platelets to the ‘injury site’, but in this scenario, these platelets are not helpful because they can form a blockage and stop blood flow. This is the main cause of a heart attack. And this is also why some of you at risk of a cardiac event may be on blood thinners.
Recently a new medication that helps reduce inflammation, low-dose colchicine (LoDoCo), was approved by the FDA to lower the risk of cardiac events in those with high inflammation.
Related Topics
Red Yeast Rice vs Statins for High Cholesterol
Red yeast rice has been used in traditional Chinese medicine for centuries. In recent years, its use as a natural alternative to statins has become more popular with some small studies suggesting the red yeast rice supplements may be effective in reducing cholesterol levels.
Learn moreFamilial Hypercholesterolemia (FH)
Familial hypercholesterolemia (FH) is a genetic disorder that affects the body's ability to remove low-density lipoprotein (LDL) cholesterol from the bloodstream, leading to elevated cholesterol levels. Approximately 1 in 250 individuals are affected by it, but only about 10% are aware they have it.
Learn moreImportant Cholesterol Markers You Should Know About
The CDC estimates that approximately 38% of Americans have unhealthy total cholesterol levels of 200 mg/dL or higher, but what does that mean?
Learn moreTop 3 Supplements For High Cholesterol
When you are diagnosed with high cholesterol, certain foods and supplements can help lower cholesterol levels. Keeping your cholesterol at healthy levels is important to reduce the risk of heart attack and stroke.
Learn moreCholesterol and Inflammation
While cholesterol may be the "fuel" for a heart attack or stroke to occur, inflammation may be the trigger that causes it to happen.
Learn moreUnderstanding CRP and Cholesterol as Markers of Heart Disease Risk
C-reactive protein (CRP) and cholesterol are both markers of heart disease risk, and their relationship to inflammation in the body. While cholesterol is a major risk factor for heart disease, high levels of CRP can indicate inflammation in the body, which can also contribute to the development and progression of heart disease.
Learn more




