Osteoporosis - Symptoms, Diagnosis & Treatment
What is Osteoporosis?
Osteoporosis, also referred to as porous bones, is a medical condition that causes your bones to become weak and fragile, causing you to be more susceptible to fractures (hip, wrist, and/or spine).
Your bone is a living tissue that undergoes continuous deterioration and replacement. Osteoporosis develops when the production of new bone is insufficient to counteract the loss of existing bone.
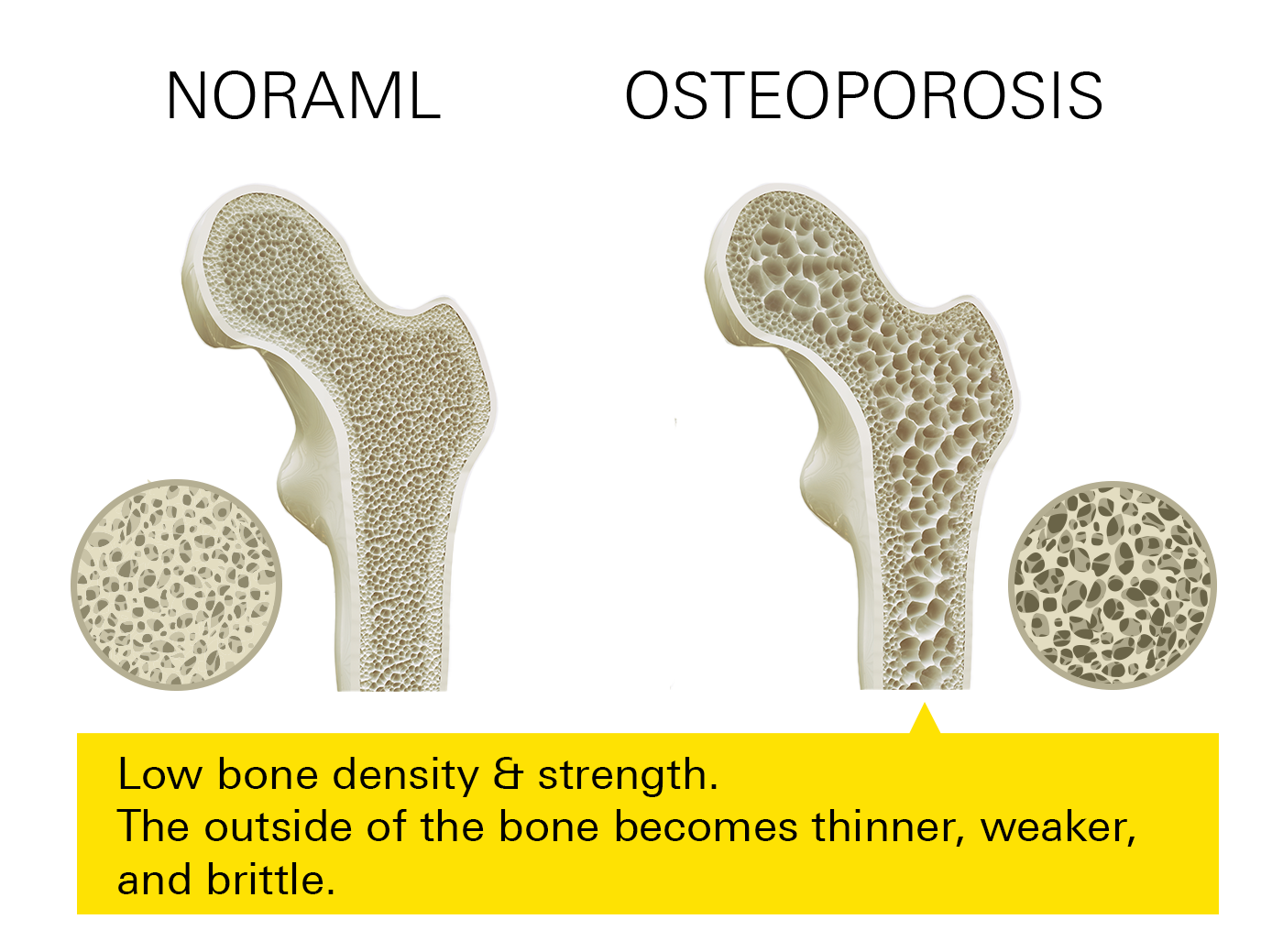
A healthy bone has compact holes throughout. These holes get larger as a result of osteoporosis, which reduces your bone's density and strength. The outside of your bone also becomes thinner, weaker, and brittle.
What are the symptoms of osteoporosis?
Osteoporosis typically shows no symptoms. This medical condition is often referred to as a “silent sickness” for this particular reason. However, some signs and symptoms that you should look out for include:
- Loss of height over time—getting shorter by an inch or more
- Change in posture, stooped or bending forward
- Weaker grip strength
- Lower back or neck pain that’s often caused by a fractured or collapsed vertebra
- Bone fractures—are often caused by a fall.
- A bone that breaks much more easily than expected
- Receding gums—if your jaw is losing bone, your gums may regress.
- Shortness of breath due to smaller lung capacity that’s caused by compressed disks
- Weak and brittle fingernails
Who is at risk of developing osteoporosis?
This condition can affect both men and women of all races. However, osteoporosis is most common in postmenopausal women. The risk is greatest for Caucasian and Asian women, particularly older women who have passed menopause.
Common factors and conditions that are at a higher risk of osteoporosis include:
- Advanced age
- Your body begins to break down bones faster than it’s able to replace them when you’re in your 30s.
- Women and men often lose bone at the same pace by the time they are 65-70 years old.
- Caucasians and Asians are at a higher risk of developing osteoporosis
- You may be at a higher risk of developing osteoporosis if your parents and/or grandparents have displayed any symptoms of the condition, such as a hip fracture following a minor fall.
- Women are much more likely to develop osteoporosis than men.
- Because they have less bone to lose than individuals with more body weight and larger frames, individuals that are severely restricting food intake, are underweight, and/or are petite and skinny are more likely to develop osteoporosis.
- Menopause, which occurs around the ages of 45-50 years, may accelerate bone loss in women because of the altered hormone levels it causes.
- Such as inflammatory bowel disease (IBD), celiac disease, gastric bypass, and malabsorption syndromes.
Diagnosing osteoporosis
Osteoblasts are the cells involved in bone formation. Osteoclasts are the cells involved in bone resorption and break down tissue in your bone. By analyzing your bone density, your doctor may be able to diagnose osteoporosis.
Your bone health is evaluated by measuring your bone mineral density (BMD). The gold standard test to measure BMD and diagnosis of osteoporosis is a dual-energy X-ray absorptiometry (DEXA, or DXA). This measures the BMD of your spine and hip and calculates a T-score or a Z-score.
If a DXA is not available, your doctor may use an ultrasound. Ultrasound readings provide bone density in 1 location; if it’s low, then individuals are encouraged to receive a DXA scan.
Since vertebrae fractures are common in older individuals, and usually lack symptoms, vertebral imaging may be done if height loss is observed or if BMD testing indicates osteopenia (low bone density, but has not yet progressed to osteoporosis).
Preventing osteoporosis
- Exercise: Individuals with low bone density should perform regular weight-bearing exercises, such as walking and/or jogging, as well as muscle-strengthening exercises, such as weight training and/or yoga.
- Preventing falls: If your bone density is low, care must be taken to avoid falls. Factors that put individuals at an increased risk of falls include a history of recent falls, medications that cause sedation/sleepiness, or orthostasis (low blood pressure that occurs when standing up) (i.e. hypertension medications, sedatives, hypnotics, etc). Preventing falls requires measures to improve muscle strength, balance, and vision.
Common ways to prevent falls include:
- Wearing corrective lenses
- Safe shoes (I.e. nonslip shoes, and socks)
- Wearing appropriate clothing that will not cause falls
- Keeping rooms brightly lit
- Removing clutters from areas where you walk
- Using a cane or a walker
- Calcium: Adequate calcium intake is required throughout your life. Calcium consumption is critical in children, in pregnancy, when the fetus can deplete the mother’s stores, and during the years around menopause when bone loss is rapid. Dietary calcium intake is preferred, with supplements used if needed.
Adults generally require approximately 1,000–1,200 mg of calcium daily. Consider taking calcium supplements if you have trouble getting enough calcium from your diet.
Foods that are rich in calcium:
- Broccoli
- Low-fat dairy products, such as milk, yogurt, and cheese
- Salmon with bones
- Kale
- Dark greens and leafy vegetables
- Vitamin D: Vitamin D is required for calcium absorption, and low levels could result in various health conditions, such as autoimmune disease and cancer.
Sunlight exposure for 10–15 minutes daily, 2–3 times a week while wearing sunscreen, can increase the production of vitamin D.
Adults generally require approximately 400–600 IU (international units) of vitamin D daily. Individuals 70 years or older require approximately 800 IU daily.
Foods that are rich in vitamin D:
- Egg yolks
- Salmon
- Swordfish
- Fortified milk
- Orange juice
What are treatment options for osteoporosis?
Medication to support bone density development is part of the treatment for osteoporosis.
Bisphosphonates
Taken orally this drug class of medications is the first-line option for the treatment and/or prevention of osteoporosis in most individuals
Bisphosphonates increase your bone density by inhibiting osteoclast activity (cells that break down calcium in your bones) and bone resorption. They decrease both vertebral and hip fracture risk.
Alendronate (brand: Fosamax, Binosto)
- For prevention of osteoporosis in postmenopausal women: 5 mg daily or 35 mg weekly
- For treatment of osteoporosis in both postmenopausal women and men: 10 mg daily or 70 mg weekly
Risedronate (Actonel, Atelvia)
- For prevention and treatment of osteoporosis: 5 mg daily, 35 mg weekly, 75 mg on two consecutive days per month, or 150 mg monthly
- For treatment of osteoporosis in men: 35 mg weekly
Ibandronate (Boniva)
- For prevention and treatment of osteoporosis: 150 mg monthly (taken on the same date every month)
Side effects of these medications include:
- Calcium deficiency
- Phosphorous deficiency
- Abdominal pain
- Indigestion
- Nausea
- Vomiting
- Difficulty and/or discomfort swallowing
- Heartburn
Warning: Bisphosphonates may cause osteonecrosis of the jaw (ONJ), which is a medical condition in which an area of your jawbone is not covered by the gums, making it difficult to heal. Due to this risk, dental work should be done prior to starting treatment.
Drug interactions: Bisphosphonates should be separated from calcium, iron, and magnesium supplements for at least 2 hours.
Estrogen agonist/antagonists containing products
These medications are used orally to treat osteoporosis in postmenopausal women. They are not for use in men.
Raloxifene (Evista): 60 mg daily
- This medication is a selective estrogen receptor modulator (SERM) and decreases bone resorption.
- Raloxifene is used for the prevention and treatment of osteoporosis in postmenopausal women
- Side effects
- Hot flashes
- Leg cramps/muscle spasms
- Swelling that occurs in your lower legs or hands
- Joint pain
- Flu symptoms
- Infections
- This medication has a black box warning (the strictest warning against prescription medications that carry a serious safety risk) for increasing the risk of death due to a stroke in women who are at risk for coronary events, such as venous thromboembolism (VTE- blood clots that occur in your veins).
Conjugated estrogens/Bazedoxifene (Duavee): 1 tablet (0.45/20 mg) daily
- This medication is used for the prevention of osteoporosis in postmenopausal women with a uterus.
- Side effects:
- Nausea
- Diarrhea
- Abdominal pain
- Muscle spasms
- This medication has a black box warning (the strictest warning against prescription medications that carry a serious safety risk) for causing endometrial cancer.
Calcitonin
This medication is a nasal spray that works by inhibiting bone resorption by osteoclasts. It’s less effective than other agents for the treatment of osteoporosis, and with long-term use, calcitonin may increase your risk of developing cancer.
Calcitonin (Miacalcin): 1 spray (200 units) in one nostril daily
Side effects:
- Back pain
- Muscle aches/pain
- Nausea
- Dizziness
Parathyroid hormone (PTH)
These mediations are subcutaneous (SC) injections (injected under all the layers of your skin) that are analogs of human parathyroid hormone, which works by stimulating osteoblast activity and increasing bone formation.
They are used for the treatment of osteoporosis when there is a very high risk of fractures.
Because of safety issues associated with the long-term use of these medications, the general duration of treatment is restricted to 2 years or less.
Teriparatide (Forteo): 20 mcg SC daily (must keep refrigerated)
Abaloparatide (Tymlos): 80 mcg SC daily (must keep refrigerated)
Side effects:
- Joint pain
- Leg cramps
- Nausea
- Dizziness
Speak With Your Doctor
Osteoporosis can be uncomfortable and painful for many individuals. There are a variety of things you can do to prevent and treat osteoporosis, from maintaining a healthy diet and exercising regularly to using the right medication for you.
Talk to your healthcare provider today and send your prescription to Marley Drug. Save up to 95% compared to your local pharmacy by using Marley Drug.