- Atherosclerosis is a condition where arteries thicken and narrow due to plaque buildup inside their walls. This plaque, made of fats, cholesterol, calcium, and inflammatory cells, restricts blood flow over time, making arteries less flexible.
- Risk factors include older age, family history of early heart disease, high cholesterol, high blood sugar, high blood pressure, tobacco use, and sedentary habits.
- Often develops silently for years or decades. Symptoms arise when blood flow is significantly reduced, leading to chest pain, shortness of breath, leg pain during exercise, or signs of stroke (weakness, speech issues). Sometimes the first sign is a heart attack or stroke.
- Management involves lifestyle changes, medications, and medical procedures to improve blood flow in severely narrowed arteries and reduce the risk of complications.
- Preventing atherosclerosis focuses on managing modifiable risk factors through regular monitoring and management of blood pressure, cholesterol, and blood sugar. It also includes avoiding all tobacco products, maintaining an active lifestyle, following a balanced diet, and getting routine medical checkups for early detection of risk factors.
Overview
Atherosclerosis is a condition characterized by the thickening and narrowing of arteries caused by the plaque inside the artery walls. This plaque is made of fats, cholesterol, calcium, inflammatory cells, and other substances found in the blood. Over time, this buildup causes the arteries to become narrower and less flexible, limiting blood flow.
Impact on Life
The narrowing and hardening of arteries mean that organs and tissues do not receive the oxygen and nutrients to function properly. Over the long term, this can lead to organ damage, heart attacks, or strokes.
Atherosclerosis doesn't only affect the heart and brain. It can cause problems in other areas where arteries are present, including the legs (leading to peripheral artery disease), kidneys, or the formation of aneurysms. Before a serious event occurs, atherosclerosis can cause chronic chest pain (angina), shortness of breath, or limit mobility.
Atherosclerosis is often a silent process that begins early in life and progresses over decades. You might not experience any symptoms until a significant blockage or a sudden event occurs. This makes it particularly insidious because you might not know it's developing until it has already caused considerable damage.
Stable vs. Unstable Plaque
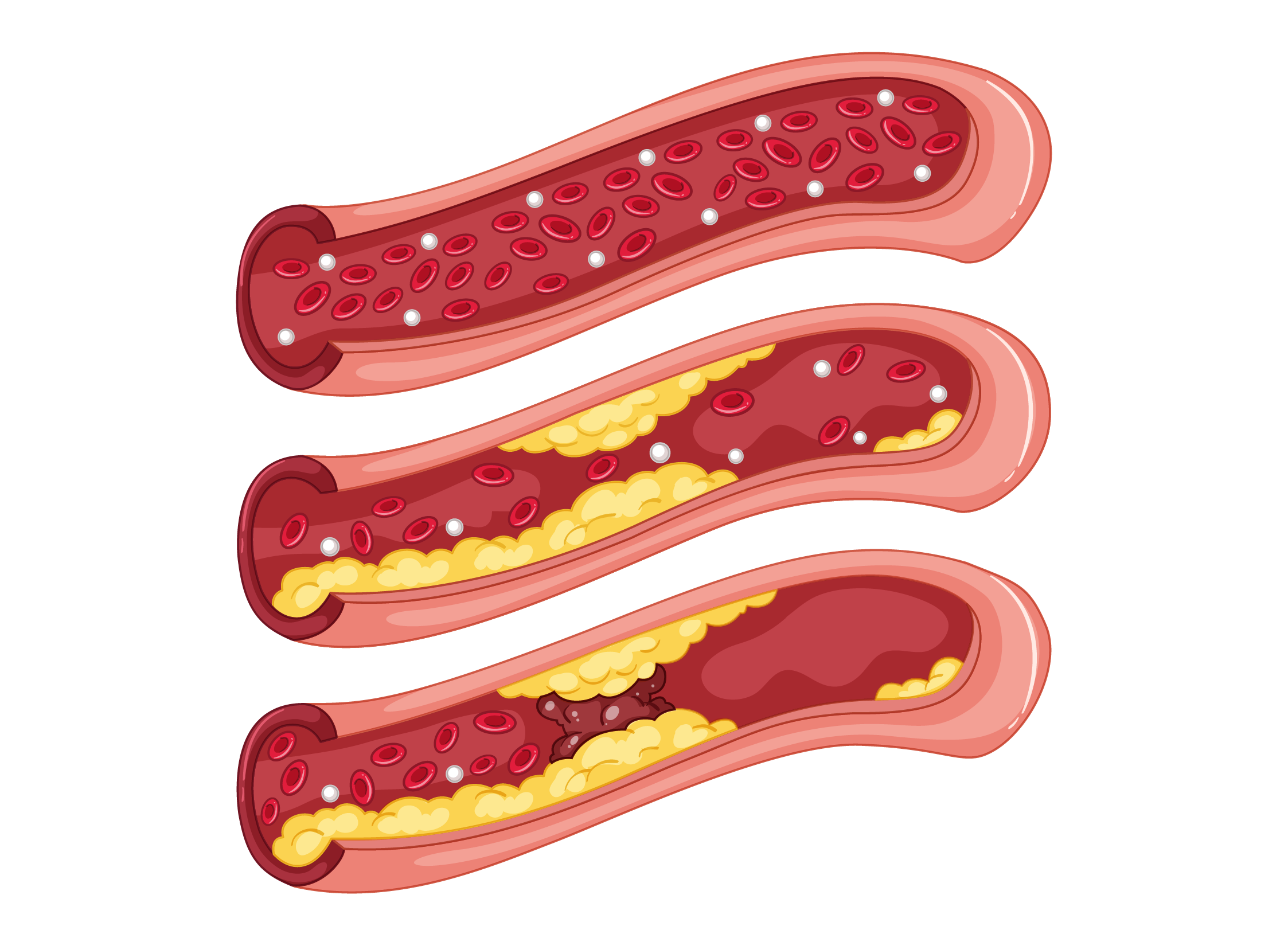
Not all plaques behave the same way. Some plaques are stable, growing slowly over many years. Others are vulnerable or unstable with a significant risk of rupturing.
When a plaque ruptures, the body initiates a healing process by forming a blood clot. If this clot grows large enough to completely block the artery, it can lead to a heart attack or a stroke, depending on the location of the blockage.
Prevalence
According to the Centers for Disease Control and Prevention (CDC), heart disease, which often results from atherosclerosis, is the leading cause of death for men and women in the United States. In 2022, approximately 702,880 Americans died from heart disease, accounting for about 1 in every 5 deaths.
The prevalence of atherosclerosis increases with age, but it's important to note that the process can begin early in life. Studies have shown that the beginnings of atherosclerosis can be found in children and teenagers, especially those with risk factors including obesity, high blood pressure, and high cholesterol.
Causes
How Plaque is Formed
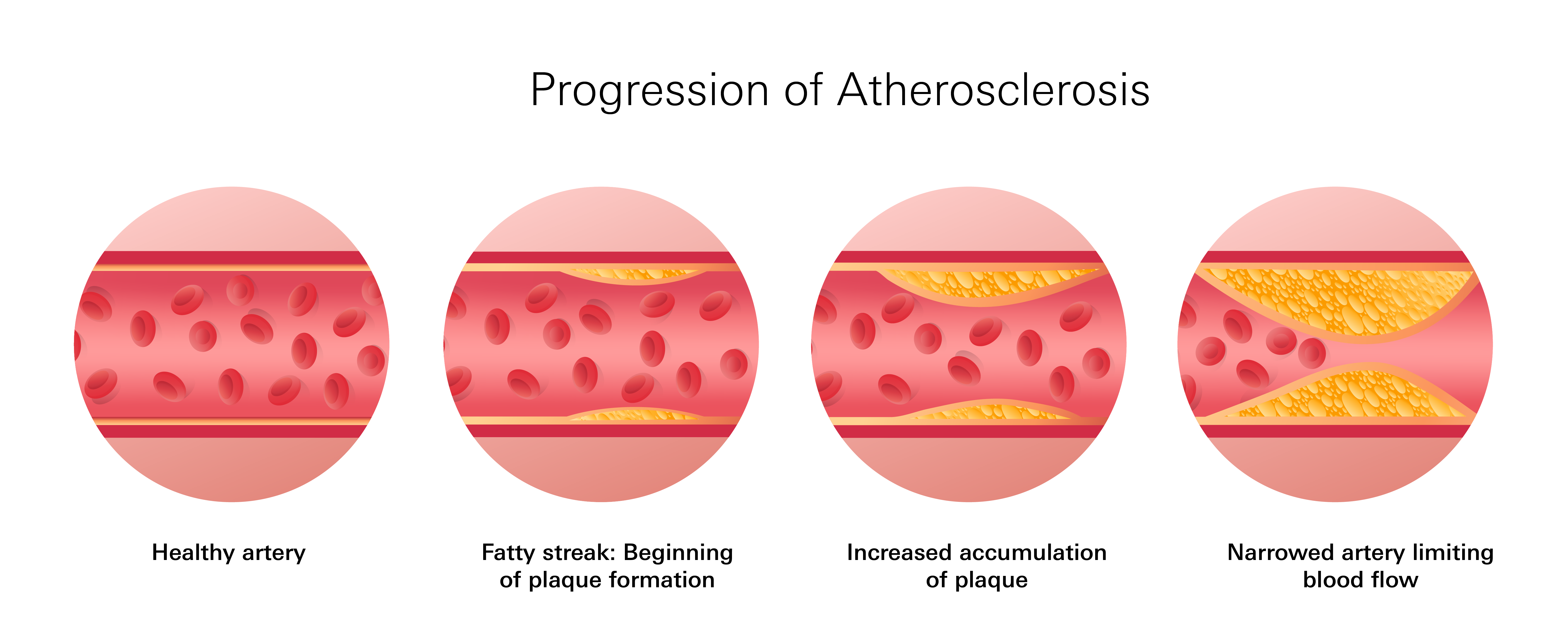
The process of atherosclerosis begins when the inner lining of arteries called the endothelium becomes injured. This damage can occur gradually due to conditions like blood pressure, elevated LDL cholesterol, smoking, diabetes, and long-term inflammation in the body. This damage acts as a gateway, allowing LDL cholesterol to enter the artery wall.
Inflammation and Plaque Growth
Once LDL cholesterol enters the artery wall, it triggers an inflammatory response. Your body sends white blood cells to the area, treating like an injury. These immune cells attempt to clear the cholesterol. Unfortunately, this process leads to more cells being added to the plaque.
What starts as a small fatty streak can gradually turn into a larger, hardened plaque. As this plaque expands, it narrows the artery and interferes with blood flow. This reduced flow means less oxygen and fewer nutrients can reach the tissues and organs.
Risk Factors
Atherosclerosis is a slow process that often unfolds over decades, affected by how your arteries respond to ongoing physical stress, inflammation, and various other factors. The longer these stressors persist, the greater the likelihood of damage to your artery walls, making it easier for cholesterol to become trapped beneath their inner lining and initiate plaque formation.
So, what exactly increases this stress on your arteries? It's often a combination of several factors:
Age
As we age, our arteries naturally tend to become stiffer and less flexible. This reduced elasticity makes them less able to handle changes in blood pressure. This stiffness can create an environment where cholesterol is more easily lodged in the artery walls, setting the stage for plaque development.
These age-related changes often become more noticeable in men after age 45 and in women after age 55.
Family History
If you have a parent, sibling, or child who developed heart disease at a relatively young age, you may have an increased risk. This suggests that inherited traits can influence how your arteries respond to cholesterol, how your body processes fat, and how likely your immune system is to create inflammation, all of which matter when it comes to plaque development.
High Blood Sugar
Elevated blood sugar levels, whether due to diabetes or insulin resistance, have a significant impact beyond just glucose control.
Excess sugar in the bloodstream can irritate and damage the inner lining of the arteries, making them more reactive to circulating fats.
Over time, this internal damage creates an environment that attracts LDL ("bad") cholesterol, leading to the formation of plaque.
High Blood Pressure
Elevated blood pressure doesn't just put a strain on your heart; it also physically stretches and weakens the walls of your arteries, making them more susceptible to damage and plaque buildup.
Tobacco Use
Whether it's cigarettes, vaping, or other forms of tobacco use, it directly harms your blood vessels.
Tobacco interferes with the delivery of oxygen to your tissues. It worsens inflammation throughout the body. It also makes platelets (blood cells involved in clotting) stickier, increasing the likelihood of blood clots forming around unstable plaque.
Sedentary Lifestyle and Weight Gain
A lack of regular physical activity, especially when combined with weight gain, reduces your body's ability to effectively regulate blood pressure and blood sugar levels.
Without regular movement, your circulation becomes less efficient. This can make your blood vessels more prone to stiffness and accelerate the accumulation of plaque.
Types and Symptoms
The location of this plaque determines which type of atherosclerotic disease develops. Although the underlying mechanism is the same, the complications and symptoms vary depending on which arteries are affected.
Carotid Artery Disease: Affects the Brain
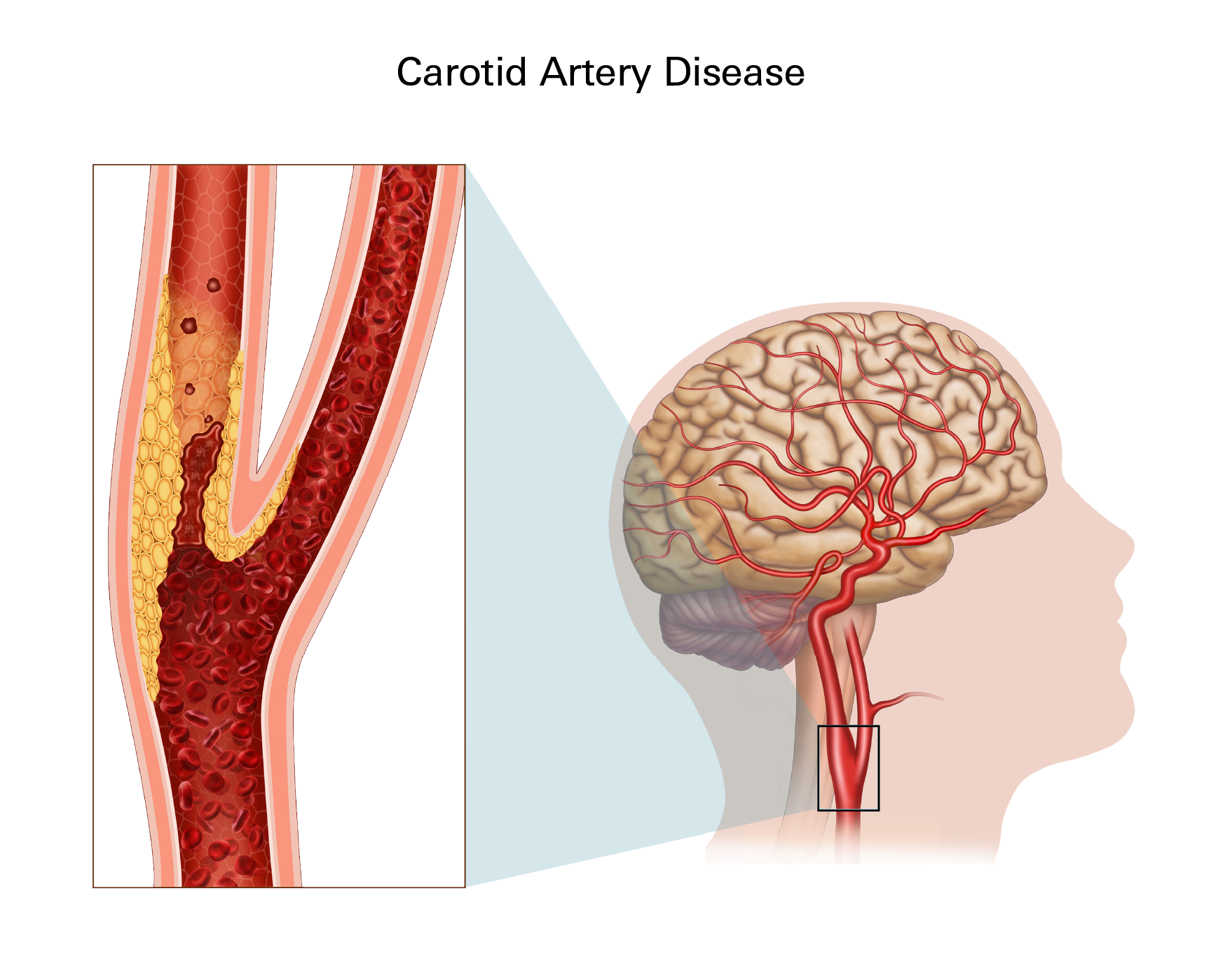
Carotid artery disease occurs when plaque accumulates in the arteries on either side of your neck that supply blood to your brain.
If these arteries become severely narrowed, it can reduce the delivery of oxygen to your brain. This increases your risk of stroke or transient ischemic attacks (mini-strokes).
Symptoms
- Sudden weakness or numbness, typically on one side of the body (face, arm, or leg)
- Difficulty speaking or slurred speech
- Trouble understanding speech
- Sudden vision loss or blurring, especially in one eye
- Dizziness, lack of coordination, or balance problems
- Severe headache with no clear cause
Coronary Artery Disease (CAD): Affects Heart's Vessels
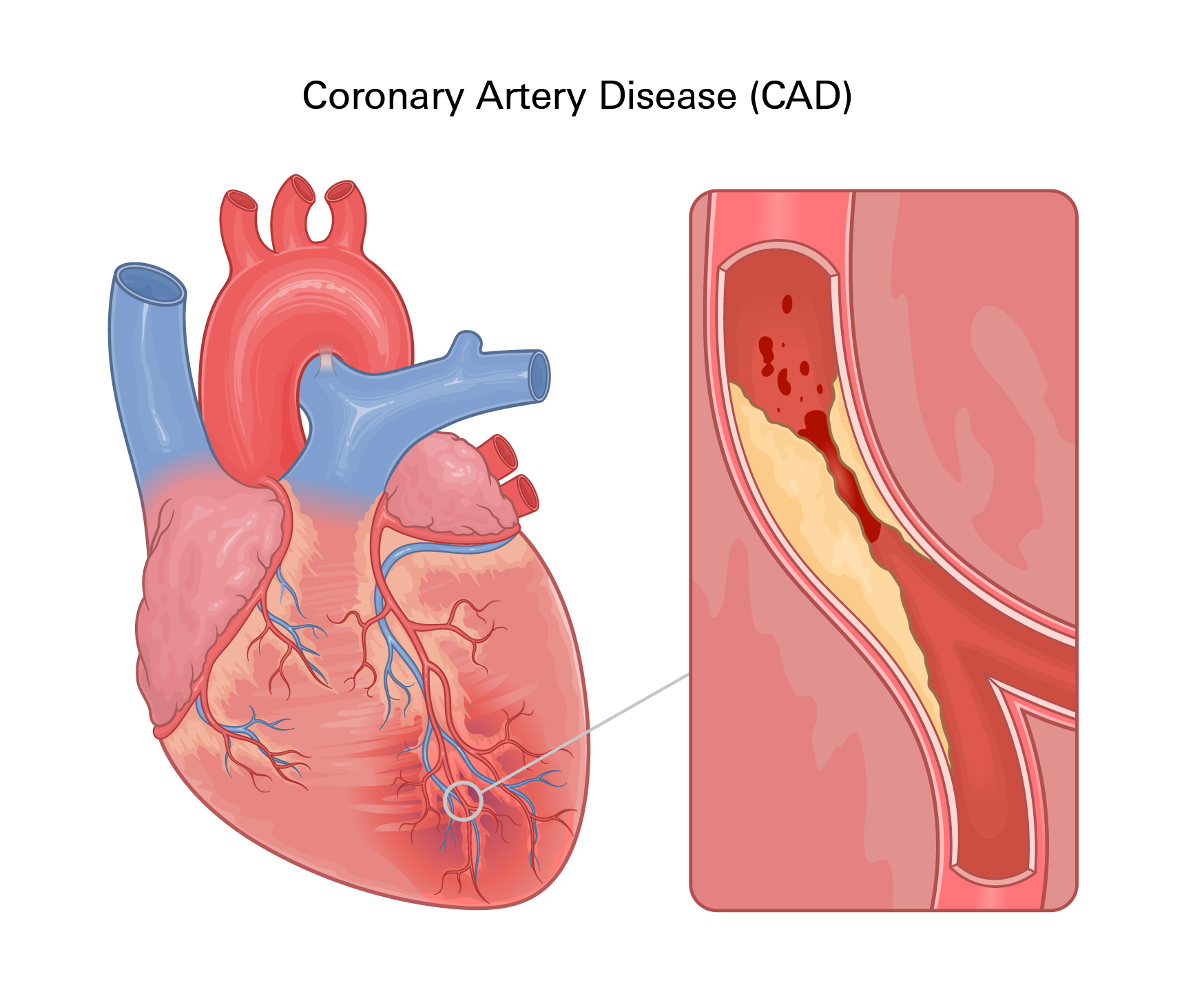
Coronary artery disease is one of the most well-known forms of atherosclerosis. It affects the arteries that supply blood to your heart muscle. This can lead to chest pain, fatigue, shortness of breath, or, in severe cases, a heart attack.
Symptoms
- Chest pain or pressure (angina), triggered by physical activity or stress
- Shortness of breath
- Fatigue during exertion
- Heart palpitations or an irregular heartbeat
- Pain radiating to the arm, shoulder, jaw, neck, or upper back
- Nausea, sweating, or dizziness, especially during a heart attack
Peripheral Artery Disease (PAD): Affects Limbs and Pelvis
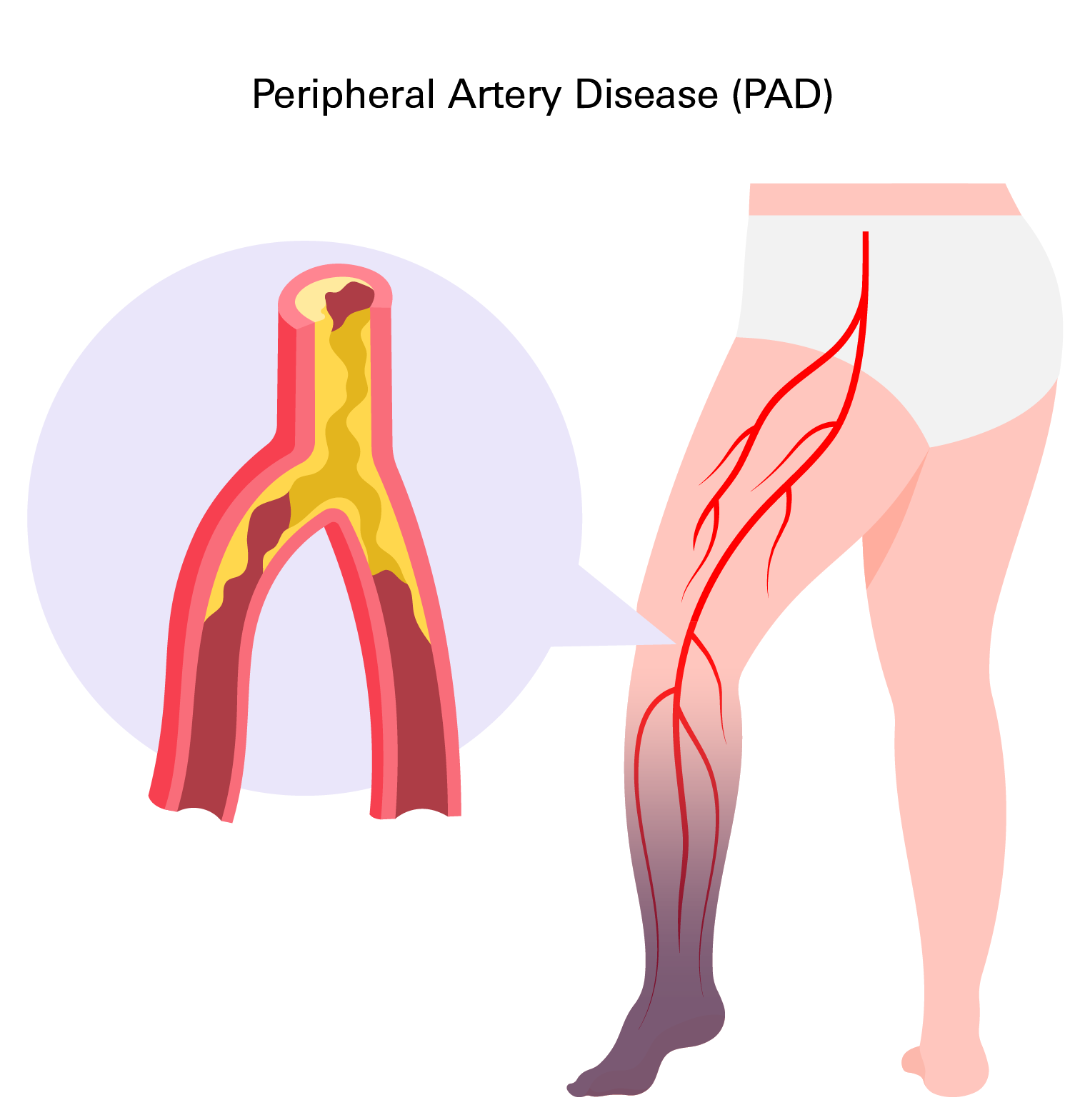
Peripheral artery disease typically involves the arteries in your legs, although it can also affect the arteries in your arms or pelvis.
As blood flow to your limbs becomes restricted, you may experience pain, especially during walking. You might also notice that wounds on your legs or feet take longer to heal. In advanced cases, PAD can lead to tissue damage and ulceration.
Symptoms
- Pain, cramping, or tiredness in the legs or hips while walking (claudication)
- Pain in the legs or feet at rest, especially at night
- Coldness or numbness in one leg or foot
- Sores on the toes, feet, or legs that are slow to heal
- Weak or absent pulse in the legs or feet
- Skin that looks pale, shiny, or bluish
Renal Artery Stenosis: Affects the Kidneys
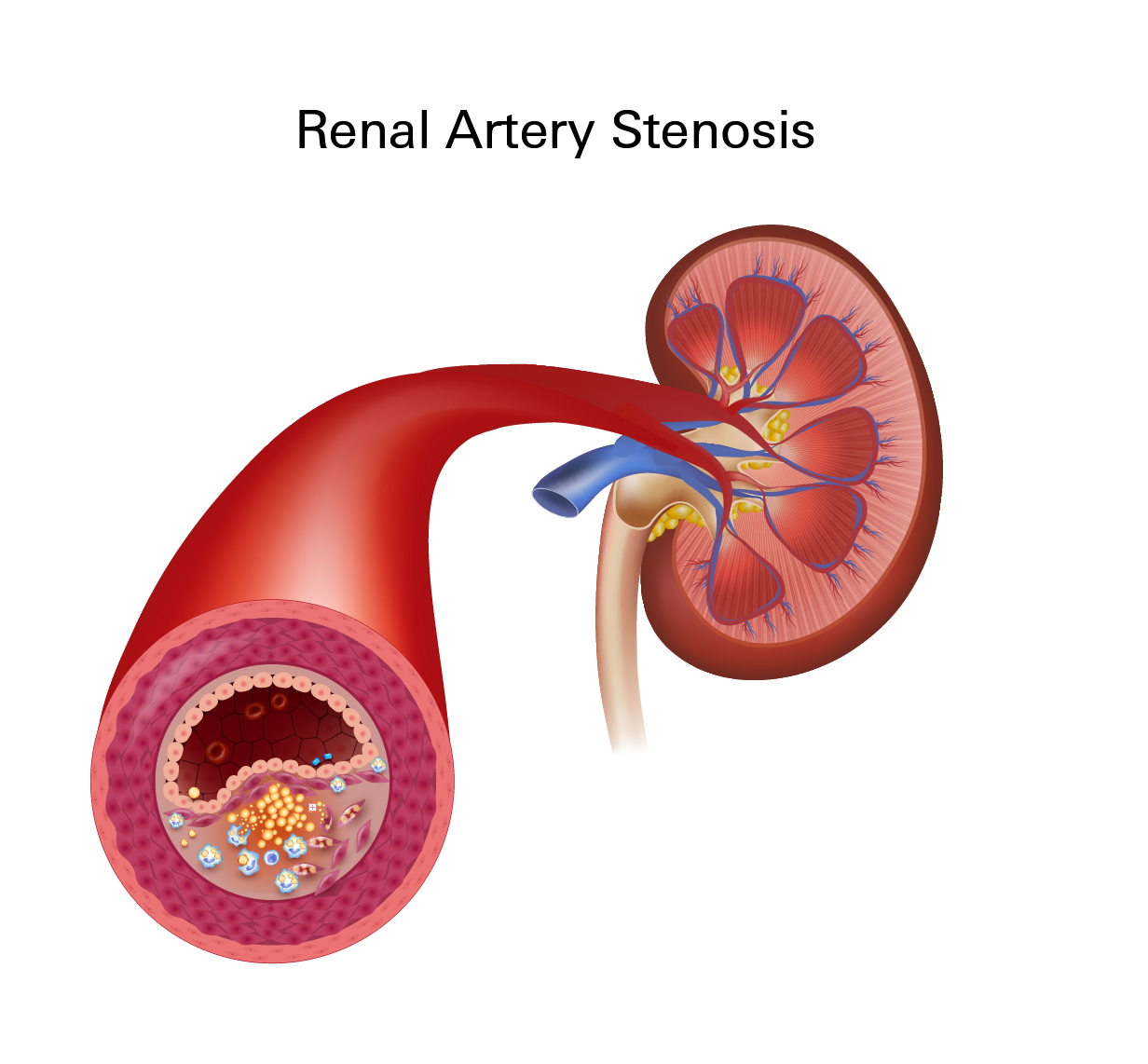
Renal artery stenosis refers to the buildup of plaque in the arteries that supply blood to your kidneys. This can contribute to uncontrolled high blood pressure or progressive kidney damage.
Symptoms
- High blood pressure that does not respond well to standard treatment
- Gradual decline in kidney function, often detected through lab tests
- Swelling in the legs or ankles (in more advanced cases)
Vertebral Artery Disease: Affects the Back of the Brain
Vertebral artery disease involves plaque accumulation in the arteries that deliver blood to the back part of your brain.
This area of the brain controls vital functions such as breathing, heart rate, and coordination. Reduced blood flow here can lead to dizziness, coordination problems, or stroke.
Mesenteric Artery Ischemia: Affects Intestines
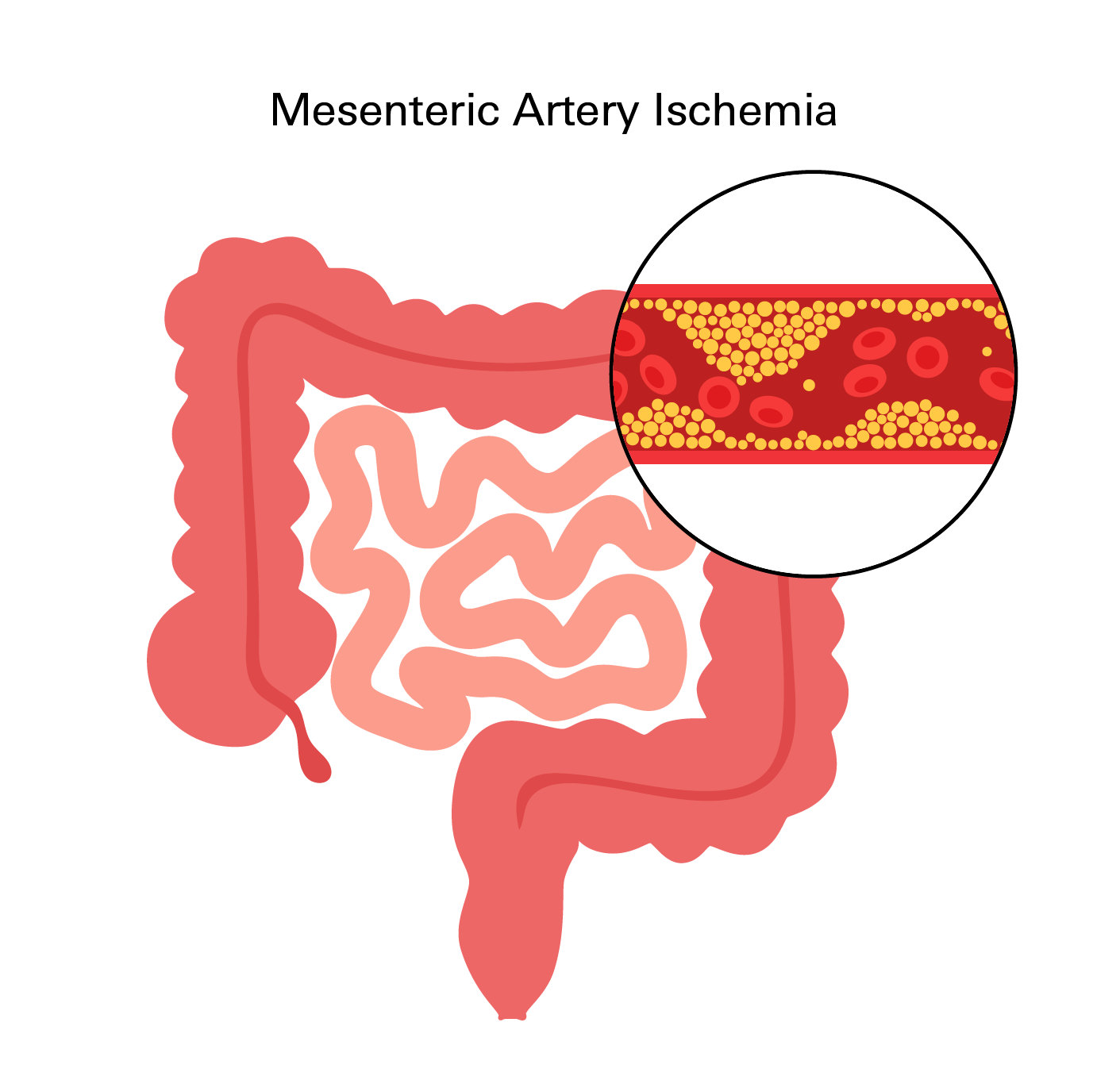
Mesenteric artery ischemia develops when plaque builds up in the arteries that carry blood to your intestines. This can lead to abdominal pain, especially after eating, due to an inadequate blood supply during digestion. In severe cases, it may result in damage to the intestinal tissue.
Symptoms
- Abdominal pain that begins shortly after eating
- Fear of eating due to post-meal discomfort
- Nausea, bloating, or changes in bowel habits
- Unexplained weight loss
Important Note: Atherosclerosis can affect multiple areas of your body simultaneously, leading to overlapping or gradually evolving symptoms. In some instances, the first noticeable sign of atherosclerosis is a serious event like a stroke or heart attack. Therefore, it is crucial to seek immediate medical attention for any new, sudden, or unexplained symptoms, particularly those involving your heart, brain, or circulation. Early recognition and intervention can significantly improve outcomes and potentially prevent more severe complications down the line.
Diagnosis
Because atherosclerosis often develops silently, individuals may not be diagnosed until signs of reduced blood flow appear or after experiencing a cardiovascular event. However, with appropriate screening and follow-up, earlier detection is possible.
The Diagnostic Process
The process typically begins with a detailed medical history. Your healthcare provider will ask about symptoms like chest pain, leg pain during walking, or shortness of breath.
They will also review your personal and family history of conditions that increase the risk of atherosclerosis, including heart disease, high blood pressure, high cholesterol, diabetes, and smoking.
During the physical exam, your provider may listen for abnormal sounds (bruits) in your arteries, which can indicate turbulent blood flow through narrowed vessels.
They may also check for weak or absent pulses in your limbs, differences in blood pressure between your arms and legs, or signs of poor circulation such as cold skin, slow-healing wounds, or changes in skin color.
Blood Tests
These look for cholesterol levels, blood sugar, inflammation markers, and kidney function. Elevated cholesterol or blood sugar can indicate an increased risk, even in the absence of symptoms.
Electrocardiogram (ECG or EKG)
This test records the electrical activity of your heart and can detect signs of previous heart damage or reduced blood flow to the heart muscle.
Stress Testing
This involves monitoring your heart while you exercise (on a treadmill or stationary bike). If you cannot exercise, medication can simulate the effects. The goal is to see how well your heart functions under stress, which can reveal blockages in the coronary arteries.
Ankle-Brachial Index (ABI)
This non-invasive test compares blood pressure in your ankles to the blood pressure in your arms. Lower blood pressure in the legs can indicate peripheral artery disease.
Ultrasound
Ultrasound uses sound waves to create images of blood vessels and measure how fast blood is flowing. It is often used to evaluate the carotid arteries in the neck, the arteries in the legs, or the abdominal aorta.
CT Angiography or MR Angiography
These imaging studies allow providers to look directly at the arteries to identify areas of narrowing or plaque buildup. A contrast dye is used to highlight the blood vessels for clearer imaging.
Cardiac Catheterization and Coronary Angiography
This invasive test is used when coronary artery disease is strongly suspected. A thin tube is inserted into a blood vessel and guided to the heart, where dye is injected into the coronary arteries to visualize blockages in real time using X- rays.
Treatment
Treating atherosclerosis involves more than just managing the plaque that has already formed. The main goal is to slow the progression of the disease, reduce your risk of serious complications, and improve blood flow to the areas of your body affected.
Treatment generally combines lifestyle changes, medications, and, in more advanced cases, procedures to restore circulation.
Atherosclerosis is a chronic condition that usually requires long-term management. Each component of your treatment plan will be tailored to your specific risk factors, the extent of the disease, and whether you have already experienced complications like a heart attack, stroke, or blood flow problems.
Lifestyle Modifications
Before discussing medications, it's important to understand that certain habits have a direct effect on how quickly atherosclerosis develops. Improving daily routines can significantly slow plaque buildup and sometimes even help stabilize existing plaque so it's less likely to cause complications.
Recommended lifestyle modifications include:
- Heart-Healthy Diet: Eat foods rich in fiber, unsaturated fats, and antioxidants. Reduce or eliminate processed meats, excess sodium, fried foods, and sugary drinks.
- Regular Physical Activity: Exercise helps improve blood flow, lower blood pressure, and regulate blood sugar. Even moderate activity, like consistent walking, can make a significant difference.
- Quitting Tobacco: Smoking directly damages your arteries and accelerates the growth of plaque.
- Stress Management: Chronic stress can elevate blood pressure and worsen inflammation.
- Healthy Body Weight: Reaching and maintaining a healthy weight can improve cholesterol levels, reduce blood pressure, and help regulate blood sugar.
These changes are often started early in treatment, whether or not medications are prescribed. In many cases, lifestyle changes alone are not enough to fully control the disease, which is where medications come in.
Medications
Medications play a key role in treating atherosclerosis because they help control the underlying conditions that cause or worsen plaque buildup.
- Cholesterol-Lowering Medications (Statins): These are among the most frequently prescribed treatments. Statins effectively reduce LDL ("bad") cholesterol, which is a primary driver of plaque formation.
- Blood Pressure Medications: These medications help reduce the strain on your artery walls.
- ACE Inhibitors: Help relax blood vessels and may offer additional protection to your kidneys.
- Beta Blockers: Reduce the workload on your heart and are particularly beneficial after a heart attack.
- Calcium Channel Blockers: Help blood vessels relax and lower blood pressure.
- Symptom Management:
- Nitrates: These medications temporarily widen the arteries, improving blood flow to your heart muscle and relieving chest pain.
- Ranolazine: This medication can help relieve chest discomfort, especially when symptoms are not adequately controlled by other drugs.
- Diabetes Medications: For patients with both diabetes and atherosclerosis, medications that effectively regulate blood sugar are crucial. Better glucose control directly reduces the long-term risk of plaque development.
- Clot-Dissolving Agents (Thrombolytics): These powerful medications may be used in emergency situations to dissolve existing blood clots that are blocking blood flow and causing a stroke, heart attack, or organ ischemia.
Prevention
Preventing atherosclerosis starts with protecting your arteries before damage occurs. While this condition often progresses silently, research shows that early lifestyle changes and risk management can significantly reduce your risk of serious complications.
Studies have shown that maintaining healthy cholesterol levels, managing blood pressure and blood sugar, avoiding tobacco, and staying physically active can slow the progression of atherosclerosis and lower your risk of heart attack and stroke.
Some prevention strategies may include the following:
- Manage blood pressure, cholesterol, and blood sugar through regular monitoring, diet, exercise, and medications when needed.
- Avoid smoking and tobacco use, as even occasional exposure harms the blood vessels.
- Stay physically active with regular movement to support circulation and metabolic health.
- Follow a balanced eating pattern, rich in whole grains, fruits, vegetables, lean proteins, and healthy fats, while limiting salt, sugar, and processed foods.
- Get routine checkups, even if you feel well, to catch early signs of imbalance that may affect your arteries.
While genetics and age cannot be changed, studies show that many of the key drivers of atherosclerosis can be modified with time and consistency. The earlier the intervention begins, the more impact it can have in preserving long-term cardiovascular health.
Related Topics
Cholesterol: What It Is and Why You Should Care
Cholesterol is a waxy substance found in your blood that comes from either your liver or from the foods you eat such as meat, dairy and processed foods. Not all cholesterol is bad; your body uses some of it to help make cells, hormones and vitamins, but it is possible to have too much.
Blood Thinners Don’t Really “Thin” Blood
Blood thinners, also known as anticoagulants, are medications that help prevent the formation of blood clots. They are commonly used to treat conditions involving the risk of blood clots, such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and certain heart conditions.
Which DOAC Is Best for You
DOACs are a newer type of blood thinners that prevent blood clots and treat conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as to prevent stroke in people with atrial fibrillation.
Why is it important to manage your blood pressure?
If blood pressure is elevated for too long it puts strain on the body and can lead to several serious and permanent health complications and conditions