- Biliary dyskinesia is a gallbladder condition where bile doesn’t flow properly, often causing pain after meals.
- The primary symptom is biliary colic, which is pain in the upper right abdomen, often triggered after eating fatty, heavy meals.
- Diagnosis involves symptom review, blood tests, and a HIDA scan to check gallbladder function.
- Treatment includes diet changes, medications, and surgery to remove the gallbladder if symptoms persist.
Overview
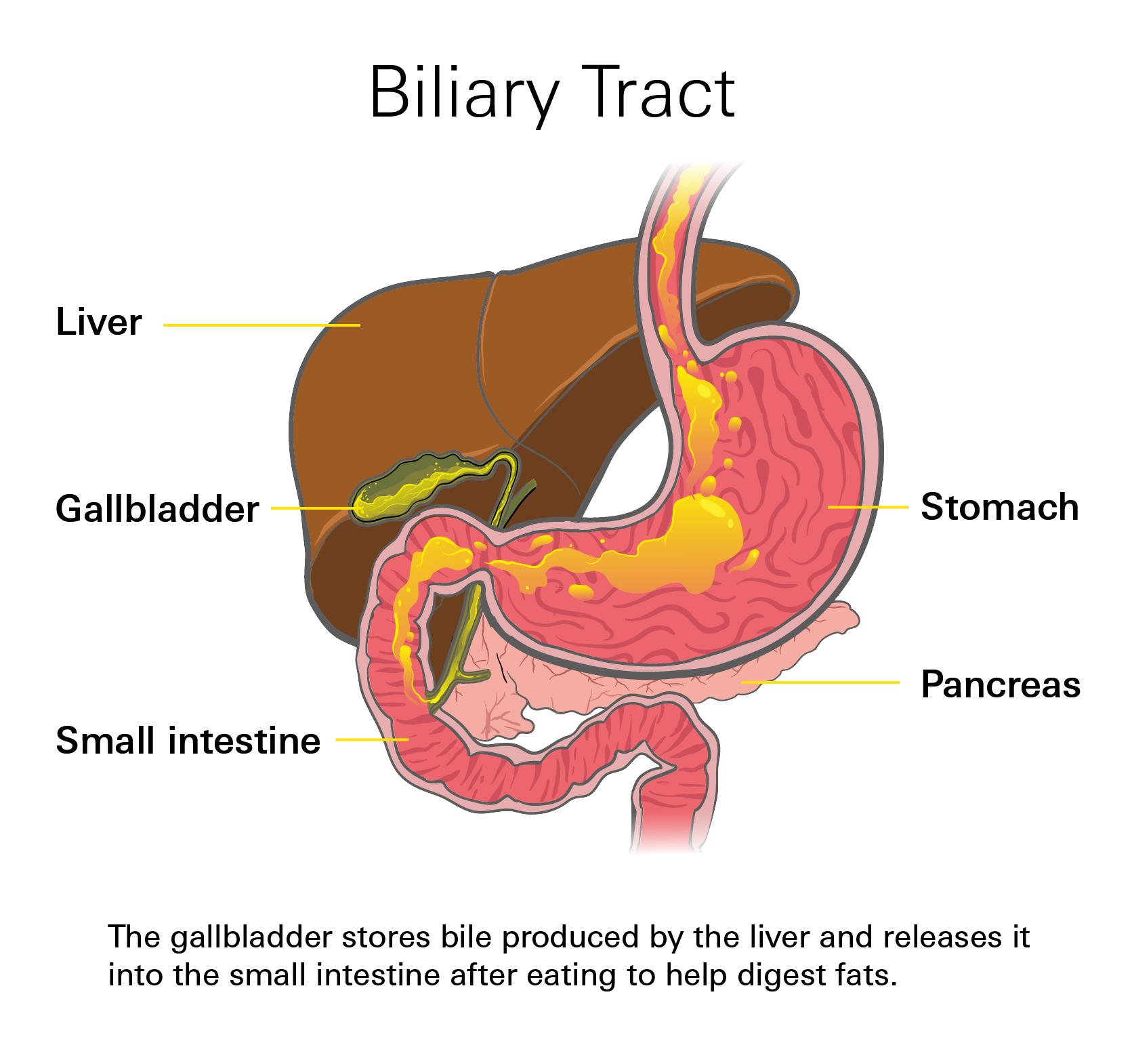
Biliary dyskinesia is a condition where the gallbladder and bile ducts do not move bile properly. Bile is a fluid made by the liver to help digest fats. It is stored in the gallbladder and released into the small intestine when you eat.
Normally:
- The gallbladder squeezes to push bile out.
- A small muscle called the sphincter of Oddi opens to let bile flow through the bile duct and closes to keep it in place.
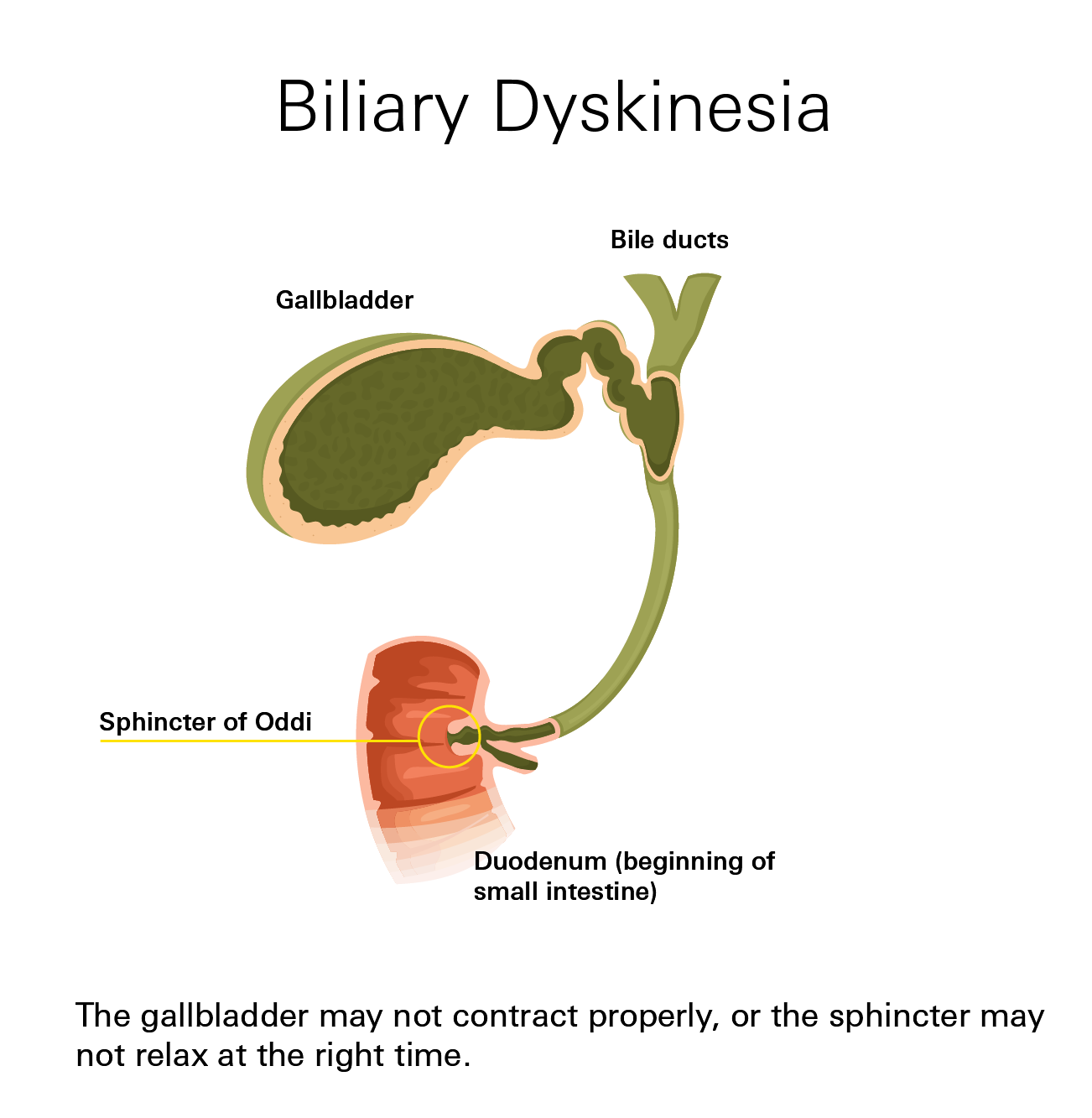
In biliary dyskinesia, this process is poorly coordinated. The gallbladder may squeeze weakly, or the sphincter may not relax at the right time.
This causes bile to drain slowly or back up, leading to pressure and pain in the upper right abdomen. Nausea after meals (especially fatty ones) is also common.
The gallbladder may look normal on scans, but it does not empty bile correctly or at the right time. This can happen with or without gallstones.
Types
There are two main types, based on whether gallstones are present:
- Acalculous (no stones): Also called functional gallbladder disorder. The gallbladder does not contract well, even though scans look normal. The muscle may be weak or not get the right signals. Bile stays trapped, causing pain or fullness after eating.
- Calculous (with stones or sludge): Gallstones or thick bile make it harder for the gallbladder to empty normally. This worsens symptoms even if stones do not fully block the duct.
How Common Is It?
Biliary dyskinesia is still uncommon but diagnosed more often now due to better tests and awareness. In the U.S.:
- From the early 1990s to early 2010s, gallbladder removals for this condition nearly doubled (from ~40 to ~90 cases per million people per year).
- It is now seen more in children and teens than in the past.
- It affects women more than men, most often between ages 20–40.
Exact numbers of people living with it are unclear, but improved imaging helps catch it earlier.
Symptoms
The main symptom is pain in the upper right abdomen called "biliary colic" (under the ribs, where the gallbladder sits). Pain may spread to the center of the belly or right shoulder and often starts after eating fatty or fried foods.
Other common symptoms:
- Dull, cramping pain that comes and goes
- Nausea or vomiting after meals
- Feeling bloated or overly full
- Loss of appetite
- Burping or gas, especially after eatingm
- Discomfort with greasy foods
Pain may last minutes to hours and can worsen at night or after large meals.
Seek emergency care (call 911) if you have:
- Severe, constant, or sharp pain
- Fever or chills
- Yellowing of the skin or eyes (jaundice)
- Repeated vomiting
- Swollen or hard abdomen
These can signal infection or a blocked bile duct. For most people, symptoms are mild and come and go, but see a doctor to prevent worsening.
Risk Factors
The exact cause of biliary dyskinesia is not fully known. It’s believed to be related to a problem with the complex signals between the nerves, muscles, and hormones that control the digestive system’s movement.
Common Risk Factors
While it can affect anyone, biliary dyskinesia is most often seen in:
- Women, especially ages 20–40
- Older adults (gallbladder function slows with age)
- People who are overweight or have rapid weight changes
- Those with a family history of gallbladder disease
- People with gallstones or Sludge
- Patients with Irritable Bowel Syndrome (IBS) or other gut motility issues
- Those with hormonal changes (pregnancy, certain birth control pills)
Stress and irregular eating may contribute but are not proven.
Diagnosis
There is no single test that confirms biliary dyskinesia. Doctors use a step-by-step approach with your symptoms, exam, and tests.
Medical History and Physical Exam
Your doctor asks about
- Pain location, timing, and triggers (like fatty foods)
- How long episodes last
- Other symptoms (nausea, bloating)
Blood Tests
These tests check your liver enzymes and other chemical levels. Normal results here often help confirm that your liver and bile ducts aren't inflamed or blocked by stones, which points toward a problem with function (dyskinesia).
Imaging and Functional Tests
- Ultrasound: Looks for gallstones, sludge, or gallbladder swelling. Usually the first imaging test.
- CT or MRI: Used if ultrasound is unclear; rules out other causes of pain.
- HIDA Scan (most important for diagnosis): A safe tracer is injected. A camera tracks how well the gallbladder fills and empties. Poor emptying (<35–40%) supports the diagnosis.)
- Upper Endoscopy (EGD): A thin camera checks the stomach and upper intestine to rule out ulcers, reflux, or other issues mimicking gallbladder pain.
Diagnostic Criteria (Common Patterns)
Doctors typically diagnose biliary dyskinesia when:
- You have recurring pain in the upper right abdomen lasting >30 minutes
- Pain disrupts daily activities
- Symptoms do not improve with antacids or position changes
- Blood tests are normal
- No gallstones seen on imaging
- HIDA scan shows poor gallbladder emptying
Treatment
Treatment focuses on relieving symptoms and improving bile flow. The plan depends on how severe your symptoms are.
Lifestyle and Medication
- Diet Changes: Many find relief by avoiding foods that trigger their symptoms. This includes cutting back on fried, greasy, or high-fat meals, which force the gallbladder to contract vigorously. Eating smaller, more balanced meals may also help.
- Medication: Ursodiol (or ursodeoxycholic acid) is a medication that can help manage bile flow and, in some cases, help dissolve small stones or sludge.
Over-the-counter pain relievers may be used for mild, occasional pain flares.
Surgery: Gallbladder Removal (Cholecystectomy)
If symptoms persist, gallbladder removal (Cholecystectomy) often recommended. It is minimally invasive and highly effective.
- The surgeon makes a few small cuts (incisions) in the abdomen.
- They use a special camera (laparoscope) to see inside.
- The gallbladder is carefully detached and removed through one of the small incisions.
Most people go home the same day or within 24 hours. Mild soreness, gas, or loose stools can occur for a few days. Most patients return to regular activity within one to two weeks.
Success Rate: Studies show that 80% to 90% of patients experience significant, long-term relief from their pain and nausea after the gallbladder is removed.
Complications
If the gallbladder is not emptying properly over time, the stagnant bile can thicken and cause other problems.
- Gallstones (Cholelithiasis): Poor drainage can lead to the formation of small, hard deposits (stones) or thick sludge.
- Gallbladder Infection (Cholecystitis): If the bile build-up causes persistent inflammation, it can turn into a serious infection requiring immediate treatment.
- Blocked Bile Ducts: Stones or swelling can block the ducts, causing severe pain and jaundice.
- Pancreatitis: In rare cases, bile can back up into the duct leading to the pancreas, causing a very painful and dangerous inflammation of that organ.
Prevention
There’s no guaranteed way to prevent biliary dyskinesia, but you can lower your risk by keeping your gallbladder healthy.
- Eat regular meals. Don’t skip them
- Choose smaller portions instead of large, heavy meals
- Limit fried and fatty foods
- Maintain a healthy, steady weight
- Stay active and move throughout the day
- Drink plenty of water
If you have thyroid disease, IBS, or a history of gallstones, regular checkups are important since these conditions can affect bile flow.
You may not be able to prevent biliary dyskinesia completely, but taking care of your digestive health early can reduce strain on the gallbladder and help avoid complications later.
Related Articles
Gallstones
Gallstones are hardened deposits in the gallbladder, often made of cholesterol, that can cause no symptoms or trigger a painful "gallbladder attack."
Read more gallstonesAcid-Related Conditions: GERD and Peptic Ulcer Disease
Peptic ulcer disease (PUD) refers to painful sores, or ulcers, that develop in the lining of the stomach (gastric ulcer) or the first part of the small intestine, called the duodenum (duodenal ulcer).
Read more on GERD and Peptic UlcersWhat is Acid Reflux?
Acid reflux, also referred to as gastroesophageal reflux (GER), occurs when the sphincter muscle at the bottom of your esophagus doesn't work properly, and stomach acid can back up into your esophagus.
Read more about GERD