- Glaucoma is a group of eye diseases that damage the optic nerve, often from high eye pressure, leading to permanent vision loss if untreated.
- Glaucoma typically has no early symptoms or pain, making regular eye exams the only way to detect it before vision is lost.
- Risk increases significantly after age 40, particularly for those with a family history or of Black or Hispanic descent.
- Most cases are managed with daily prescription eye drops or simple laser procedures to lower eye pressure.
Overview
Glaucoma is a group of eye diseases that damage the optic nerve, the link that sends visual information from your eye to your brain. This damage often results from increased pressure inside the eye, though it can occur even at normal pressure levels.
How glaucoma develops
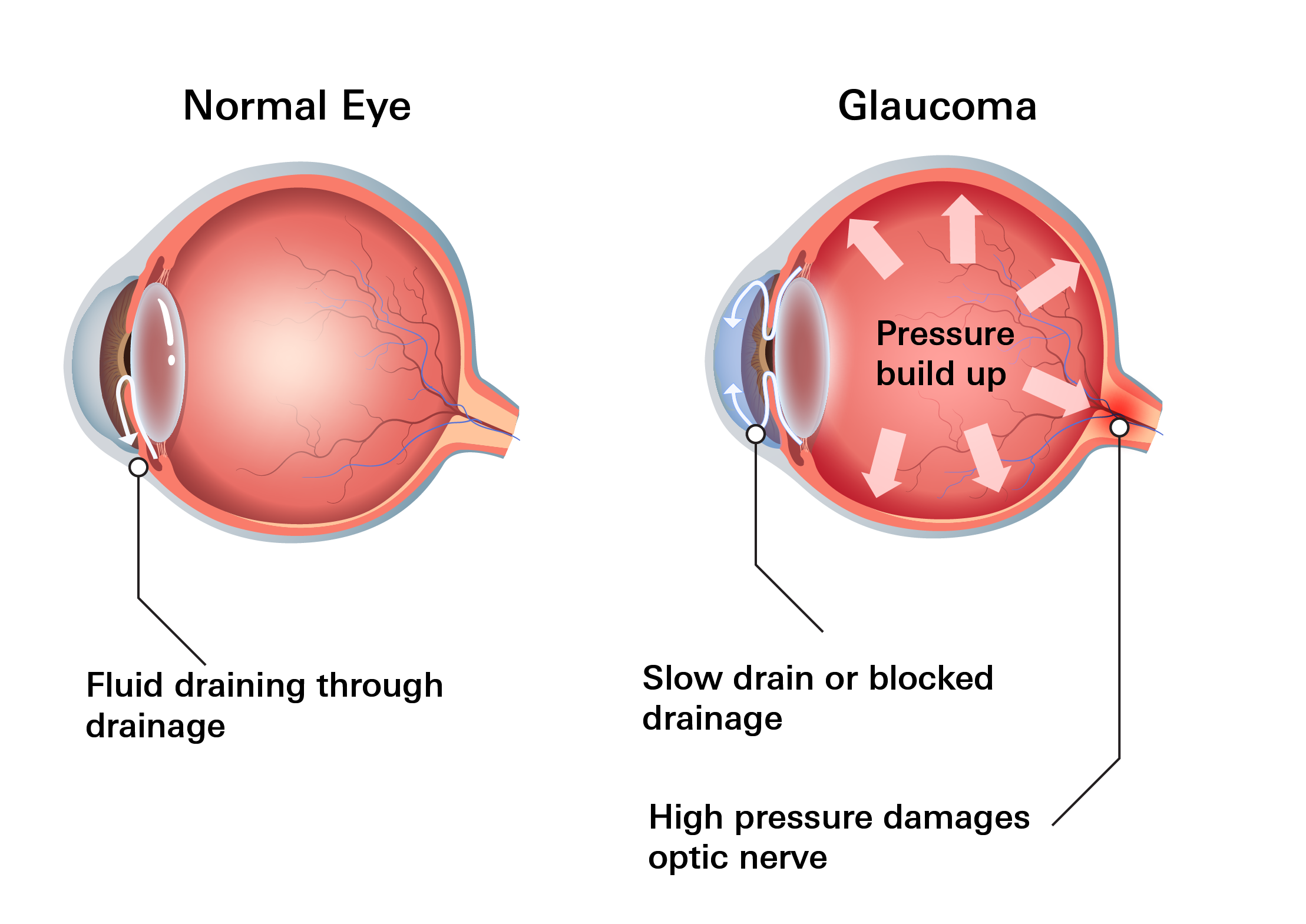
- Your eye produces a clear fluid that circulates through the front of the eye. To maintain healthy pressure, an equal amount of fluid must drain out through a microscopic drainage system.
- When drainage is blocked or too slow, fluid builds up. This buildup creates pressure that pushes against the optic nerve, killing nerve fibers and causing damage.
Early stages of glaucoma usually have no symptoms. Vision loss happens slowly and painlessly, often starting in the peripheral vision.
Many people don't notice changes until significant damage has occurred, which is why it's often called the "silent thief of sight." Vision loss from glaucoma is permanent and irreversible, but early detection through regular eye exams can help preserve remaining vision and slow progression.
How common is it?
- Glaucoma is a leading cause of blindness worldwide. In the United States, 4.22 million adults (1.62%) had glaucoma in 2022.
- Risk increases significantly after age 40 and continues to rise as you get older, reaching 5-8% in those over 65-80.
- It is more common and often more aggressive among Black and Hispanic individuals.
Regular comprehensive eye exams (pressure checks, optic nerve evaluation, visual field testing) are key for early detection, especially for those at higher risk.
Types
Glaucoma has several main types, classified as primary (no other cause) or secondary (due to another condition or injury).
- Primary open-angle glaucoma: The most common type. The drainage angle remains open, but fluid drains too slowly, causing gradual pressure buildup. No pain; side vision loss occurs first and is often unnoticed early on.
- Angle-closure glaucoma: The drainage angle narrows or becomes blocked suddenly or gradually. Pressure can rise quickly in acute cases, causing a medical emergency.
- Normal-tension glaucoma: Optic nerve damage occurs despite normal eye pressure, possibly due to poor blood flow or other factors.
- Congenital glaucoma: Rare; present at birth due to improper development of the drainage system. Babies may show cloudy eyes, excessive tearing, or light sensitivity.
- Secondary glaucoma: Caused by another eye issue or condition. Examples include:
- Neovascular glaucoma: abnormal blood vessel growth blocks drainage, often linked to diabetes or poor blood flow
- Uveitic glaucoma: inflammation interferes with drainage
- Pseudoexfoliation: flaky material builds up inside the eye and blocks drainage
- Traumatic glaucoma: develops after an eye injury, may occur years later
Symptoms
Glaucoma symptoms depend on the type and how long it has been developing. Many changes are subtle at first and can be mistaken for normal aging.
In the early stages, there are no symptoms and no pain.
1. Progressive symptoms
If you notice the following, the condition may have already progressed:
- Loss of peripheral vision: Subtle blurring or "blind spots" on the sides of your vision.
- Tunnel vision: In advanced stages, you may only be able to see straight ahead.
- Difficulty at night: Needing more light to see or having trouble driving in the dark.
- Physical signs: Bumping into furniture or door frames because you didn't see them in your side vision.
2. Emergency Symptoms (Angle-Closure)
These symptoms may come from sudden pressure changes (more common in angle-closure glaucoma). Seek immediate medical care if you experience:
- Sudden, intense eye pain or severe headache
- Nausea and vomiting
- Blurred vision or seeing "halos" (rainbow rings) around lights
- Sudden redness in the eye
Schedule an eye exam if you notice changes in side vision, have trouble navigating familiar spaces, or have difficulty driving at night.
Risk Factors
Certain traits and health conditions increase glaucoma risk:
- Family history
- Age over 40, risk increases further with age
- Elevated eye pressure over time
- Reduced blood flow to the optic nerve (low blood pressure, sleep apnea)
- Diabetes or vascular disease
- Long-term steroid use (drops, pills, or inhalers)
- Eye injury or prior eye surgery
- Severe nearsightedness or farsightedness
- Chronic eye inflammation
- Thin corneas, which may mask true pressure levels
Diagnosis
Glaucoma is diagnosed through a comprehensive eye exam performed by an ophthalmologist (eye surgeon) or optometrist (eye doctor). Since early glaucoma often has no symptoms, these tests are designed to catch early changes you might not notice yourself.
No single test diagnoses glaucoma. Doctors use a combination of assessments to evaluate eye pressure, optic nerve health, drainage, and vision fields. Regular monitoring tracks changes over time.
Common tests include:
- Eye pressure measurement: A gentle test checks the pressure inside your eyes. Higher pressure may damage the optic nerve.
- Optic nerve exam:: The doctor looks at the back of your eye to check the health of your optic nerve. Changes in its shape or color can be early warning signs.
- Visual field testing: YThis test checks your side (peripheral) vision. You’ll respond to small lights or images that appear in different spots to detect blind areas caused by glaucoma.
- Optic nerve imaging: Scans measure the thickness of optic nerve fibers. Thinner tissue can show early damage, even if vision still seems normal.
- Drainage angle exam (gonioscopy): A special lens lets the doctor see how fluid drains inside your eye. This helps identify the type of glaucoma.
- Corneal thickness measurement: 3D scan that measures the thickness of the nerve fiber layer. It can catch thinning before vision loss even begins.
No single test can diagnose glaucoma. These results are combined to give a full picture of your eye health, and follow-up exams are often needed to track changes over time.
Treatment
Treatment aims to lower eye pressure to protect the optic nerve and slow disease progression.
There are no over-the-counter treatments for glaucoma. Only prescription medications and procedures prescribed by an eye doctor can control eye pressure. Non-prescription eye drops, like artificial tears, may help with dryness but do not treat glaucoma.
Prescription Eye Drops (first-line treatment)
These are used daily (often once or twice) to improve fluid drainage or reduce fluid production.
- Prostaglandin analogs (usually first choice): Increase fluid outflow. Highly effective.
- Examples: Xalatan (latanoprost), Lumigan (bimatoprost), Travatan Z (travoprost), Zioptan (tafluprost)
- Common side effects: mild eye redness, eyelash growth, darkening of the iris, slight stinging
- Rho kinase inhibitors: Relax the drainage system in the eye to improve fluid outflow.
- Examples: netarsudil (Rhopressa)
- Common side effects: eye redness, small blood spots, blurry vision
- Cholinergic agonists: Increase drainage of fluid from the eye.
- Examples: pilocarpine (Isopto Carpine)
- Common side effects: headache near the eyes, blurry or dim vision (especially in low light), small pupils, irritation
- Alpha adrenergic agonists: Reduce fluid production in the eye
- Examples: apraclonidine (Iopidine), brimonidine (Alphagan P)
- Common side effects: dry mouth, eye redness or itching, mild dizziness, sleepiness
- Beta blockers: Lower eye pressure by reducing fluid formation
- Examples: timolol (Timoptic, Betimol, Istalol), betaxolol (Betoptic)
- Common side effects: slower heart rate, fatigue, mild burning after application, shortness of breath in people with lung disease
- Carbonic anhydrase inhibitors: Decrease fluid production inside the eye
- Examples: dorzolamide (Trusopt), brinzolamide (Azopt)
- Common side effects: unusual taste in the mouth, temporary blurred vision, mild eye discomfort, headache
Laser and Surgical Options
If eye drops don’t control pressure well or cause side effects, laser or surgical treatments may be recommended. These improve drainage or reduce fluid production.
Laser treatments
- Trabeculectomy: Creates a new pathway for fluid to drain from the eye, reducing pressure. Used when other treatments aren’t effective.
- Drainage implant surgery: Small tubes or devices are placed to help fluid escape and control pressure, often used for complex or advanced cases.
Surgical options
- Laser trabeculoplasty: Common for open-angle glaucoma. The laser helps the drainage tissue work better so fluid exits more easily. Pressure typically improves gradually.
- Laser peripheral iridotomy: Used for angle-closure glaucoma. The doctor creates a small opening in the colored part of the eye (iris) to help fluid flow and prevent sudden pressure spikes.
Prevention
There is no way to fully prevent glaucoma, as many risk factors (like age, genetics, and eye structure) can't be changed. The best "prevention" is early detection to stop damage before significant vision loss occurs. Glaucoma is often silent until advanced.
Key steps:
- Routine eye exams: Regular pressure checks, optic nerve evaluations, and visual field testing are the best ways to detect glaucoma early.
- More frequent exams if at risk: If you have a family history or past eye injury, start exams earlier and get them more often.
- Track changes over time: Long-term pressure trends help detect problems earlier than a single test result.
- Optic nerve imaging: Scans track nerve thickness and can show early damage even if pressure seems normal.
- Cautious steroid use: Steroid medications can raise eye pressure. Regular checks are important if you use them long term.
- Manage related health conditions: Controlling diabetes, blood pressure, and sleep apnea supports healthy blood flow to the optic nerve.
- Protect your eyes from injury: Use protective eyewear for contact sports, home repairs, or high-impact activities. Eye injuries can increase glaucoma risk years later.
Ongoing Care After Diagnosis
If glaucoma is already present, regular follow‑up visits are critical. Adjusting treatment early can prevent permanent vision loss. Many people maintain stable vision for years when eye pressure is well controlled—even without symptoms.
Related Topics
What Is a Diabetic Eye Exam?
Diabetes can cause a variety of eye problems because of high blood sugar levels on the blood vessels and tissues in the eyes. When blood sugar levels are consistently high, it can damage the small blood vessels in the eyes.
Read Diabetic Eye ExamCan Diabetes Increase Glaucoma Risk?
Studies show diabetes raises the risk of glaucoma. A 2017 meta-analysis of cohort studies found people with diabetes have a higher chance of primary open-angle glaucoma (POAG), the most common type. This pattern holds in recent research too.
Diabetes and GlaucomaGlaucoma is one of the leading causes of irreversible blindness, yet it often goes unnoticed until vision loss has already occurred. In the United States, approximately 4.22 million adults have glaucoma (about 1.62% of adults), with around 1.49 million experiencing vision-affecting effects. Nearly half cases remain undiagnosed.
Glaucoma and Eye HealthTimolol for Glaucoma and Ocular Hypertension
Timolol (pronunciation: tai·muh·laal) treats pressure inside the eye caused by glaucoma, ocular hypertension, hemangioma, and other eye diseases. Treating high pressure in the eye helps to prevent blindness.
Timolol for Glaucoma and Ocular Hypertension