- Pneumonia is a lung infection where air sacs fill with fluid or pus, causing cough, fever, and difficulty breathing; it is most commonly caused by bacteria or viruses.
- Symptoms vary widely from mild (walking pneumonia) to severe, and they can be different in high-risk groups like children and older adults.
- Infants, older adults, and those with chronic health issues or weak immunity are at higher risk.
- Diagnosis is based on symptoms, a physical exam, and usually a chest X-ray, with treatment determined by the specific germ causing the infection (e.g., antibiotics for bacteria).
Overview
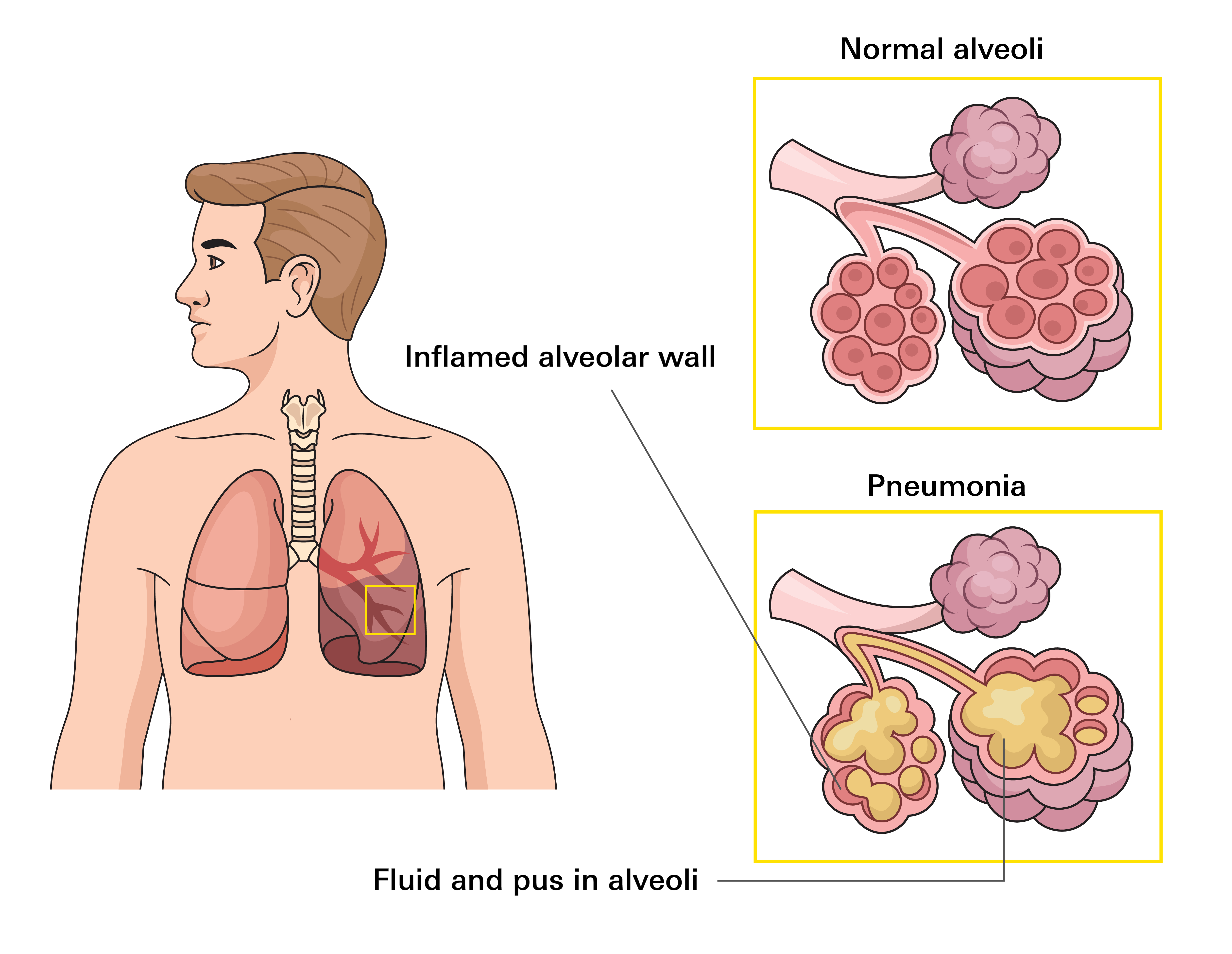
Pneumonia is a lung infection that affects the tiny air sacs in one or both lungs, called alveoli. These air sacs normally fill with air and help move oxygen into your bloodstream.
When you have pneumonia, the lining of these air sacs becomes inflamed and they fill up with fluid, pus, and immune cells. This prevents enough oxygen from getting into your bloodstream, making breathing difficult and often causing a cough and fever. The body's immune response also causes general symptoms like fatigue and aches.
Common signs include a cough (with or without mucus), fever or chills, shortness of breath or faster breathing, and chest pain that worsens with deep breaths or coughing. Symptoms can be mild or very severe.
It’s caused by bacteria, viruses, or fungi. The most common bacterial cause in the U.S. is Streptococcus pneumoniae. Viral pneumonia is often linked to flu, RSV, or COVID-19.
How common is it?
Pneumonia affects millions of people each year and is a frequent reason for clinic visits and hospital stays in the U.S. It remains a major cause of infection-related deaths.
The risk is highest for infants, older adults (age 65 and older), and people with chronic heart or lung diseases or a weakened immune system. While cases happen year-round, many causes cluster in the colder months from fall through early spring.
Types
Pneumonia is grouped based on where it starts or how it affects the lungs.
By Where It Starts
- Community-acquired pneumonia (CAP): Most common type. It starts outside hospitals, such as at home, work, or school. Can be mild or severe.
- Hospital-acquired pneumonia (HAP): Develops during a hospital stay; often more serious.
- Ventilator-associated pneumonia (VAP): Occurs in people using breathing machines; requires intensive care.
By Lung Involvement
- Single lung pneumonia: Affects one lung; severity depends on how much of the lung is involved.
- Double lung pneumonia: Affects both lungs; may cause faster oxygen drop and often needs hospital care.
Symptoms
Pneumonia symptoms can look different from person to person. They may seem mild, like a cold or flu, but they tend to last longer.
Common Signs
- Cough, with or without phlegm (thick mucus)
- Fever and shaking chills or sweats
- Shortness of breath or faster breathing than usual
- Chest discomfort that worsens when taking a deep breath or coughing
- Fatigue, low energy, and a poor appetite
- Headache and body aches
Symptoms in Specific Groups
- Older Adults (Age 65+): May have fewer or milder typical symptoms. Instead, they might show new confusion or changes in mental state, or just feel very sleepy and weak. They may also have a lower-than-normal body temperature.
- Infants and Young Children: May show signs like trouble feeding, vomiting, a grunting sound with breathing, flaring of the nostrils, or being very tired or restless.
When to Seek Medical Care
- Severe trouble breathing (struggling to speak full sentences)
- Blue or gray color on your lips or face (a sign of very low oxygen)
- New confusion, fainting, or extreme sleepiness
- Persistent high fever with shaking chills
- Chest pain that is severe or worsening
- Inability to keep fluids or medicines down, leading to signs of dehydration
Causes
Pneumonia can be caused by bacteria, viruses, or fungi. The treatment depends on the cause.
Bacteria
Streptococcus pneumoniae (most common), Haemophilus influenzae, Mycoplasma pneumoniae, Chlamydia pneumoniae
- Can follow a cold or flu. Mycoplasma often causes a milder type called "walking pneumonia."
- Legionella pneumophila causes a severe form called Legionnaires' disease and is not spread person-to-person but through contaminated water systems.
Viruses
Influenza (flu), RSV (Respiratory Syncytial Virus), SARS-CoV-2 (causes COVID-19), Human metapneumovirus (HMPV)
- Viral pneumonia is often milder, but it can be severe, and you're at risk of getting a secondary bacterial infection on top of it.
Fungi
Histoplasma, Coccidioides, Blastomyces, Pneumocystis jirovecii
- Uncommon in the general population. More likely to occur in people with weakened immune systems.
Risk Factors
While anyone can get pneumonia, certain factors increase your chance of getting it or having a more severe case.
Age and Health Conditions
- Children age 2 and younger and adults age 65 and older
- Asthma, COPD, or cystic fibrosis
- Heart failure or coronary artery disease
- Diabetes, kidney, or liver disease
- Weakend immunity due to cancer treatment, HIV, or malnutrition
- Being pregnant or in the weeks after delivery
Lifestyle and Environmental Factors
- Cigarette smoking and exposure to secondhand smoke
- Heavy alcohol use
- Swallowing or breathing issues: Conditions like stroke, Parkinson's disease, or severe reflux can make it easier to accidentally breathe in food, liquids, or vomit (aspiration), which can lead to pneumonia
- Recent illness or exposure: Flu, Covid, RSV, a hostpital stay or surgery, living in long-term facilities, use of mechanical ventilator
- Weakend immunity due to cancer treatment, HIV, or malnutrition
- Being pregnant or in the weeks after delivery
Diagnosis
Doctors begin by asking about your symptoms and medical history, followed by a physical exam and checking your vital signs. If pneumonia is suspected, they may order:
Initial Tests
- Chest X-ray: Confirms infection and shows how much of the lung is affected
- Pulse oximetry: A finger sensor checks your oxygen level
- Blood tests: A complete blood count (CBC) may show signs of infection
Further Testing (For more severe or high-risk cases)
- Viral tests: For flu, COVID-19, or RSV, especially if results would change treatment
- Sputum and blood cultures: Help identify the germ causing pneumonia, especially in moderate to severe cases
- Urine antigen test: Sometimes used to detect pneumococcal disease
- Bronchoscopy: Used to collect samples or clear thick mucus if complications are suspected
- CT scan: Offers a detailed view of the lungs to check for abscesses or fluid buildup
For mild cases in the community, a history, physical exam, oxygen check, and chest X-ray are often enough. More testing is done if symptoms are severe or risk factors are present.
Treatment
The goal of treatment is to cure the infection and prevent serious complications. Treatment is based on whether the pneumonia is caused by bacteria, a virus, or a fungus.
Targeted Medications
- Antibiotics: Used for bacterial pneumonia. The type depends on your health and severity of illness. Always finish the full course. Stopping early can cause the infection to come back and may lead to antibiotic-resistant germs. Hospital patients may receive antibiotics through an IV.
- Antivirals: Used for viral pneumonia when a treatable virus is confirmed (e.g., oseltamivir for flu, Paxlovid for COVID-19)
- Antifungals: Prescribed for fungal pneumonia (e.g., amphotericin B), less common type of pneumonia.
Supportive Care
- Rest and fluids to help your body recover
- Fever and pain relief with acetaminophen, ibuprofen, or naproxen
Note: Do not give aspirin to children or teens due to the risk of Reye syndrome - Humidified air and simple cough remedies
- Oxygen therapy if levels are low
Hospital Care
You may need to be admitted to the hospital if you:
- Have low oxygen levels
- Struggle to breathe or speak
- Feel confused or faint
- Can’t keep fluids or medicine down
- Have serious underlying health conditions
Procedures
In some cases, procedures are needed to:
- Drain fluid around the lungs
- Remove thick mucus with bronchoscopy
- Surgically remove damaged lung tissue (rare)
Prevention
The best way to fight pneumonia is to prevent it. You can significantly lower your risk by practicing good habits and staying up-to-date on vaccines.
Vaccines to Prevent Common Causes
- Pneumococcal vaccines: Recommended for: All children under 5, adults 50 and older, people 5–49 with certain health conditions (e.g., heart or lung disease, diabetes, immune suppression, smoking, alcohol use disorder)
- Flu vaccine: Every year, especially important for older adults and those with chronic conditions
- COVID-19 vaccine: Stay up to date per CDC guidance
Everyday Habits
- Wash hands often with soap and water or use alcohol-based sanitizer
- Cover coughs and sneezes with a tissue or your elbow, then wash hands
- Avoid tobacco and secondhand smoke, which weaken lung defenses
- Practice good oral hygiene and get regular dental care
- Stay home when sick to avoid spreading illness
- Clean high-touch surfaces like doorknobs and phones
- Open windows when possible and spend time outdoors for fresh air