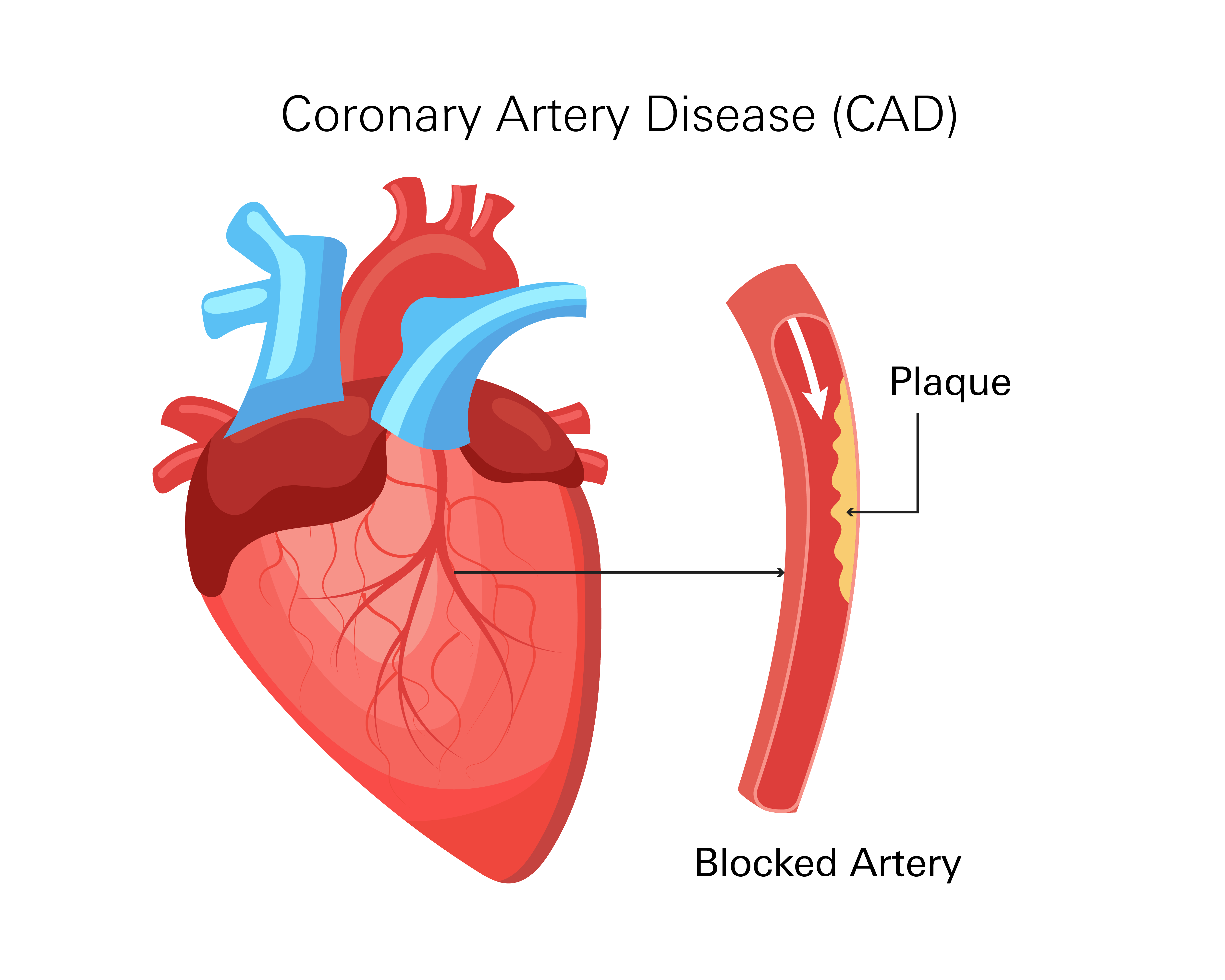
- What it is: Heart disease where arteries supplying blood to the heart narrow or block caused by plaque buildup (atherosclerosis) in the coronary arteries.
- Risk Factors: High cholesterol, high blood pressure, smoking, diabetes, obesity, inactivity, unhealthy diet, stress, family history.
- Symptoms: Often none early on. Later can include chest pain/discomfort, shortness of breath, fatigue. Heart attack can be the first sign.
- Treatment: Medications (to improve blood flow, manage cholesterol/triglycerides, prevent clots), procedures (angioplasty/stenting, bypass surgery).
- Prevention: Healthy lifestyle: control blood pressure/cholesterol, healthy diet, exercise, no smoking, manage stress/alcohol/diabetes.
- CAD is a gradual condition, early detection is important, treatment focuses on managing symptoms and preventing complications.
Overview
Coronary artery disease (CAD) is a type of heart disease that affects the arteries supplying blood to the heart. Coronary arteries deliver oxygen and nutrients for the proper functioning of the heart muscle.
When these arteries narrow or become blocked, the heart does not receive enough oxygen-rich blood. This reduced blood flow can cause symptoms like chest discomfort. In severe cases, it can lead to a heart attack.
A healthy heart depends on open and flexible coronary arteries that allow blood to flow freely. This continuous blood supply enables the heart to contract and pump blood efficiently throughout the body.
In CAD, the arteries gradually narrow due to the buildup of fatty deposits and other substances on the artery walls. This buildup restricts blood flow, forcing the heart to work harder to maintain circulation.
The reduced blood flow may not initially cause problems. However, as the narrowing progresses over time, symptoms like chest pain or shortness of breath can develop.
Sometimes, CAD is not diagnosed until a serious event occurs, such as a heart attack. A heart attack happens when blood flow to a part of the heart is completely blocked.
Because CAD develops slowly, it is considered a chronic condition. While CAD cannot always be reversed, treatment can help manage the condition and lower the risk of complications.
Prevalence
CAD is one of the most common heart conditions in the United States. The Centers for Disease Control and Prevention (CDC) reports that approximately 1 in 20 adults over the age of 20 has CAD, representing about 5% of this adult population.
Men are more likely to be diagnosed with CAD than women. Studies between 2015 and 2018 showed that around 8.3% of men aged 20 and older had CAD. For women in the same age group, it was about 6.2%.
Age is a major factor in developing CAD. While younger adults can be affected, the condition is considerably more common in older populations. Approximately 3.6% of adults aged 45 to 54 had CAD, while 9% of those between 55 and 64 were affected. The prevalence continued to increase in older age groups, with 14.3% of adults aged 65 to 74 having CAD and over 24% of those 75 and older living with this condition.
Causes
CAD develops when the coronary arteries become narrowed or blocked, reducing the flow of blood to the heart.
This occurs due to plaque buildup on the artery walls, a process called atherosclerosis. Plaque is made up of cholesterol, fat, calcium, and other substances in your blood. Over time, it hardens and makes your arteries less flexible, restricting blood flow.
Risk Factors for Plaque Buildup and Artery Narrowing
- High Cholesterol Levels: Excess LDL (“bad” cholesterol) sticks to artery walls, forming plaque, while low HDL (“good” cholesterol) makes it harder for your body to remove LDL.
- High Blood Pressure: The increased force of blood flow through the arteries can damage their inner lining over time. This damage makes it easier for plaque to accumulate.
- Smoking: Chemicals in tobacco smoke damage the lining of the arteries, accelerating the process of plaque buildup. Smoking also reduces the oxygen levels in the blood, forcing the heart to work harder.
- Diabetes: High levels of blood sugar can damage blood vessels, making them more susceptible to plaque accumulation.
- Obesity: Excess body weight is often linked to other risk factors for CAD.
- Lack of Physical Activity: A sedentary lifestyle increases the risk of developing high cholesterol, obesity, and poor circulation, all of which can contribute to CAD.
- Unhealthy Diet: Consuming a diet high in processed foods, unhealthy fats, and added sugars can increase plaque buildup.
- Chronic Stress: Long-term stress can raise blood pressure and may lead to unhealthy behaviors like smoking or overeating, indirectly increasing the risk of CAD.
- Family History: CAD can run in families.
Symptoms
CAD develops over time, and in its early stages, it may not cause any symptoms. Many patients do not realize they have CAD until their arteries become significantly narrowed. In some cases, a heart attack is the first sign of the disease.
Common Symptoms
As CAD progresses, your heart struggles to receive enough oxygen-rich blood, especially during physical activity or emotional stress. This can lead to symptoms such as:
- Chest Discomfort: A feeling of pressure, tightness, or heaviness in your chest, often triggered by exertion or stress. The discomfort may spread to your arms, neck, jaw, back, or stomach.
- Shortness of Breath: Your heart's reduced ability to pump blood can make it harder to breathe, particularly during movement.
- Fatigue: When your heart does not receive enough oxygen, it can result in an overall feeling of exhaustion, even without strenuous activity.
These symptoms may come and go, worsening over time as the condition progresses.
Serious Symptoms That Require Immediate Attention
A heart attack may occur when a coronary artery becomes completely blocked. If you experience any of these serious symptoms, seek immediate medical attention.
- Severe chest pain or pressure
- Pain radiating to the arms, jaw, neck, or back
- Cold sweats, nausea, or lightheadedness
- Sudden shortness of breath or difficulty breathing, even at rest.
Types
While CAD affects the arteries that supply blood to the heart, it can manifest differently in individuals. There are distinct types of CAD, each with unique effects on heart function and blood flow. These include:
Obstructive CAD
This is the most common form of CAD. It occurs when plaque builds up inside the coronary arteries, reducing blood flow to your heart. Over time, as your arteries narrow, your heart receives less oxygen-rich blood, which can lead to symptoms such as chest discomfort and shortness of breath. If a blockage becomes severe, it may result in a heart attack.
Non-obstructive CAD
In some cases, CAD may be present without significant blockages in your arteries. Instead of large plaque deposits, there may be smaller areas of buildup or dysfunction in the arteries that cause reduced blood flow. This type is often harder to detect because standard imaging tests may not always show major narrowing, but it can still cause symptoms and increase your risk of complications.
Microvascular CAD
This type affects the small blood vessels of your heart rather than the larger coronary arteries. The tiny vessels that branch off from the main arteries may not function properly, limiting blood flow even if the larger arteries are not significantly blocked. Patients with microvascular CAD may experience chest discomfort, especially during physical activity, even though traditional tests do not show major obstructions.
Diagnosis
Diagnosing CAD involves a combination of tests and evaluations. Your doctor will typically start by asking about your symptoms, lifestyle habits, and family history.
Blood Tests
Blood tests check for conditions that contribute to CAD. These include measurements of cholesterol, triglycerides. Blood sugar levels are also checked.
Electrocardiogram (ECG)
An ECG records your heart’s electrical activity and can help detect irregular rhythms or signs of past heart damage. If your heart has trouble receiving enough blood due to CAD, this test may show abnormal patterns. However, since CAD does not always cause rhythm changes, additional tests may be needed.
Coronary Calcium Scan
A coronary calcium scan is a type of CT scan that measures calcium deposits in the walls of your coronary arteries. The presence of calcium is a sign of plaque buildup. This test is particularly useful for patients who do not yet have symptoms but have other risk factors such as smoking or high cholesterol.
Stress Testing
Stress testing evaluates how your heart performs under physical strain. During the test, you may walk or run on a treadmill or pedal a stationary bike while your heart rate, rhythm, and blood pressure are monitored. If you are unable to exercise, medication may be used to make your heart beat faster, mimicking the effects of physical activity.
Imaging tests, such as an ECG or an ultrasound, are often used during stress testing to look for signs of reduced blood flow to the heart.
Cardiac MRI and PET Scan
A cardiac MRI provides detailed images of your heart and blood vessels, helping to detect any damage to your heart muscle or problems with blood circulation. A cardiac PET scan is another imaging test that assesses blood flow through your coronary arteries.
Coronary CT Angiography
This imaging test uses X-rays and contrast dye to take detailed pictures of your coronary arteries. It helps determine how well blood is flowing through your heart and can identify narrowed or blocked arteries.
Coronary Angiography and Cardiac Catheterization
If other tests suggest CAD is likely, a more detailed evaluation may be needed.
Coronary angiography involves injecting contrast dye into your coronary arteries using a thin tube called a catheter, which is inserted through a blood vessel. X-ray images are then taken to show any blockages or narrowing in the arteries.
This test provides the most precise information about the condition of your coronary arteries and is often used to determine if you need further treatment, such as stents or bypass surgery.
Treatment
The goal of treatment is to improve blood flow to your heart, reduce symptoms, and lower your risk of complications such as heart attacks. The specific treatment approach depends on the severity of artery narrowing, the presence of symptoms, and how well your heart is functioning.
Medications
For many patients, medications are the first choice for managing CAD. These medications work in different ways.
Improve Blood Flow and Reduce Heart Strain
- Beta-blockers, ACE inhibitors, and angiotensin receptor blockers: Help lower blood pressure and reduce the workload on your heart. Side effects may include fatigue, dizziness, or cold hands and feet.
- Calcium channel blockers: Relax your blood vessels, improving circulation and controlling blood pressure. Side effects may include swelling in your legs, dizziness, or headaches.
- Nitrates, such as nitroglycerin: Widen your coronary arteries, increasing blood flow and relieving chest discomfort. Some patients may experience headaches or low blood pressure after taking nitrates.
- Ranolazine: Used to manage chronic chest pain by improving blood flow to your heart without lowering blood pressure. It may cause dizziness, nausea, or constipation.
Manage Cholesterol and Triglycerides
- Statins: Lower LDL ("bad" cholesterol) to slow plaque buildup inside your arteries. Muscle pain or liver enzyme changes may occur in some patients.
- Non-statin cholesterol agents, including ezetimibe, PCSK9 inhibitors, and bile acid sequestrants: Used when statins alone are not enough to control cholesterol levels. Some patients experience digestive discomfort.
- Triglyceride-lowering agents, including omega-3 fatty acids, fibrates, and niacin: Help control high triglyceride levels, which can contribute to CAD. These medications may cause flushing, upset stomach, or changes in liver function.
Prevent Blood Clots
- Aspirin: A low-dose aspirin regimen may be recommended for patients at risk of heart attacks. Aspirin may increase your risk of stomach irritation or bleeding.
- Antiplatelets: Help prevent clot formation, especially after stent placement or a heart attack. Some patients may experience bruising or an increased risk of bleeding.
Medical Procedures
When medications alone are not enough to control CAD, medical procedures may be needed to improve blood flow to your heart. Some procedures include:
- Coronary Angioplasty or Percutaneous Coronary Intervention (PCI): A procedure used to widen coronary arteries that have become narrowed or obstructed due to plaque accumulation. A small mesh tube, known as a stent, may be inserted into the artery to help keep it open and reduce the risk of future narrowing.
- Coronary Artery Bypass Surgery (CABG): In cases of severe artery blockages, bypass surgery or open-heart surgery may be required. A surgeon takes a healthy blood vessel from another part of your body and attaches it to your heart, creating a new route for blood to flow around the blocked artery. This procedure restores blood supply to the heart muscle and is often used for patients with multiple blocked arteries.
Prevention
While CAD cannot always be avoided, certain habits can lower your risk or slow its progression. Keeping blood pressure and cholesterol levels controlled, following a heart-healthy diet, staying active, and quitting smoking can help protect your arteries. Managing stress, limiting alcohol, and controlling diabetes also play a role in reducing your risk of developing CAD-related complications.
If you experience chest discomfort, shortness of breath, unusual fatigue, or dizziness, it is important to talk to your doctor. Many patients do not realize they have CAD until a heart attack occurs, making early detection important. Discussing symptoms, risk factors, and testing options with your provider can help identify the condition and determine the best treatment plan.
Related Topics
Familial Hypercholesterolemia (FH)
Familial hypercholesterolemia (FH) is a genetic disorder that affects the body's ability to remove low-density lipoprotein (LDL) cholesterol from the bloodstream, leading to elevated cholesterol levels.
Read moreWhy is it important to manage your blood pressure?
You’ve probably seen countless articles about how to manage your blood pressure and products advertised as something that “helps to lower your blood pressure”, but what exactly are the risks of having high blood pressure? Alternatively, is there such thing as “too low?”
Read moreImportance of Diet and Exercise to Manage Diabetes
Managing Type 2 Diabetes typically involves a combination of medications and lifestyle changes. Most medications for T2D are designed to complement diet and exercise modifications. While medications are vital for blood sugar control, lifestyle changes are equally important to control blood sugar levels and improve insulin sensitivity.
Read more
