- Pulmonary embolism is a serious condition where a blood clot blocks blood flow to the lungs, often originating as a deep vein thrombosis (DVT) in the legs.
- Symptoms vary from shortness of breath and chest pain to fainting and blue skin, which requires immediate medical attention.
- Causes include slow blood flow due to immobility, damage to blood vessels, and underlying conditions that increase the risk of blood clotting.
- Complications can include sudden death, right heart failure due to increased strain, chronic thromboembolic pulmonary hypertension (CTEPH), and organ damage from oxygen loss.
- Treatment typically involves anticoagulation therapy (blood thinners) to prevent clot growth and new clots, with advanced treatments like fibrinolytics or thrombectomy for high-risk cases.
- Prevention includes staying active, maintaining good circulation, and using preventive measures like blood thinners or compression stockings.
Overview
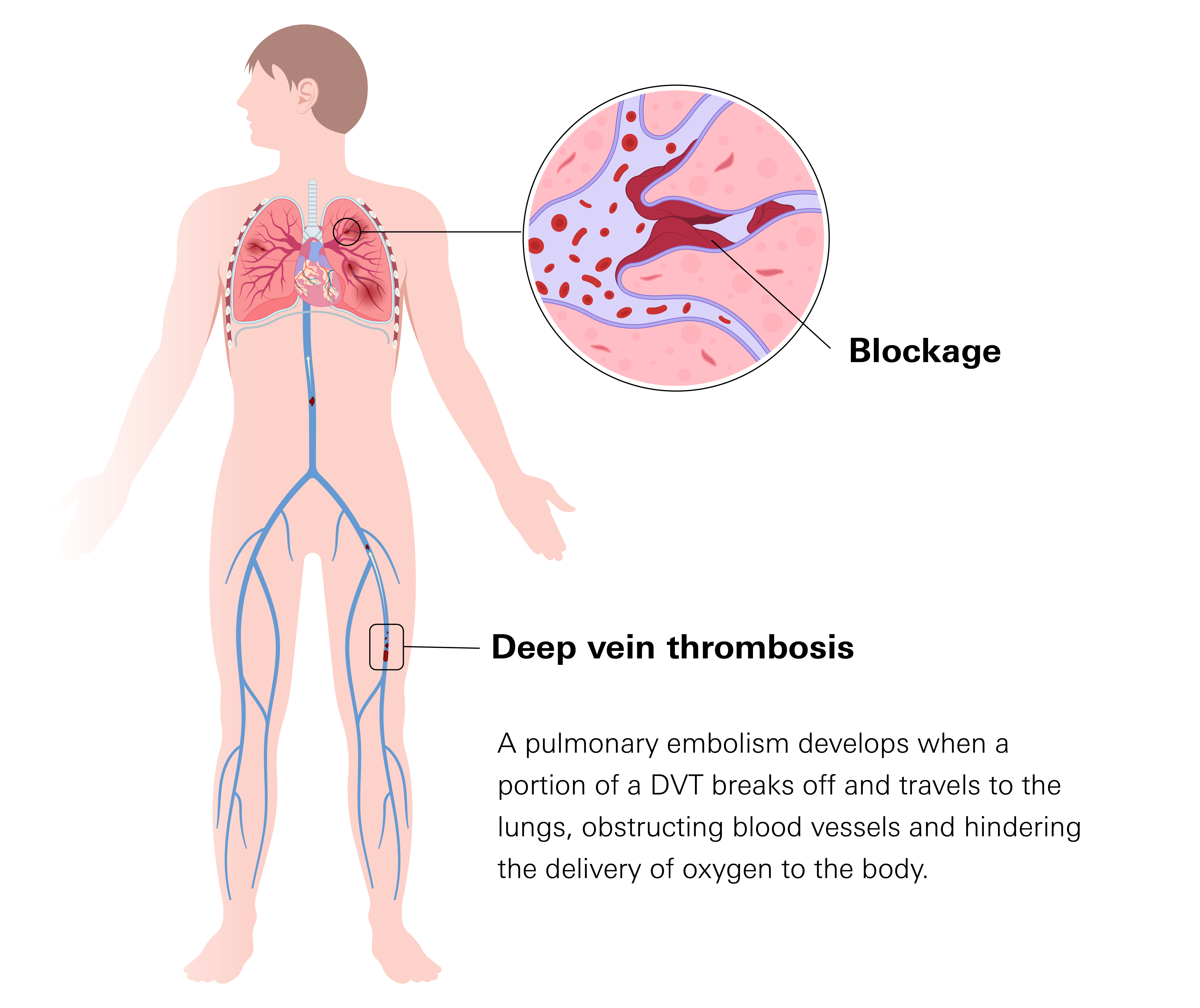
Pulmonary embolism (PE) is a serious condition that occurs when a blood clot blocks blood flow to the lungs. PE is part of a broader condition known as venous thromboembolism (VTE), which also includes deep vein thrombosis (DVT).
DVT involves the formation of a blood clot in a deep vein, typically in the legs. A PE develops when a portion of a DVT breaks off and travels to the lungs, obstructing blood vessels and hindering the delivery of oxygen to the body.
This blockage can cause sudden breathing difficulties, chest pain, and other complications. The severity of a PE varies depending on the size of the clot and the extent of the blockage, ranging from mild to life-threatening.
Prevalence
PE affects a significant number of patients in the United States each year, contributing to high rates of hospitalization, long-term complications, and deaths. While exact numbers vary, estimates suggest that approximately 370,000 cases of PE occur annually. Many of these cases are identified early and treated, but PE remains a major cause of unexpected deaths.
Studies indicate that between 60,000 and 100,000 deaths each year in the U.S. are linked to venous thromboembolism (VTE), with PE accounting for a large portion of these fatalities. In about one-quarter of PE cases, sudden death is the first sign, meaning the condition was not recognized or treated in time.
One of the most concerning aspects of PE is the risk of recurrence. According to the National Blood Clot Alliance, about 30% of patients who experience PE will develop another clot within 10 years. Additionally, PE can lead to long-term complications, such as chronic shortness of breath and increased strain on the heart.
Symptoms
PE can cause a range of symptoms, from mild discomfort to life-threatening complications. Alarmingly, in about 25% of people with PE, the first sign is sudden death. This is why understanding your symptoms is important.
Common Symptoms
Many patients experience symptoms that may seem harmless at first but can become more concerning over time. These include:
- Shortness of breath: The most common symptom. It can happen suddenly or gradually worsen over hours or days.
- Chest pain: Often described as sharp or stabbing, especially when breathing deeply. This happens because the clot irritates lung tissue.
- Cough: Some patients develop a dry cough, while others may cough up blood, which can be a sign of lung damage.
- Increased heart rate: The heart beats faster as it tries to push blood through the blocked arteries.
- Mild dizziness or lightheadedness:This can happen due to reduced oxygen levels or increased strain on the heart.
Serious Symptoms That Require Immediate Medical Attention:
- Severe shortness of breath: Sudden difficulty breathing, even at rest, may be a sign of a large clot blocking major blood flow.
- Sudden, severe chest pain: If the pain feels crushing, radiates to the shoulder, neck, or arm, or is accompanied by difficulty breathing, it could indicate heart strain.
- Fainting or loss of consciousness: This happens when blood pressure drops too low, which can occur in massive PE.
- Blue or grayish skin: A sign that the body is not getting enough oxygen.
- Weakness or confusion: In severe cases, reduced oxygen to the brain can cause disorientation or trouble thinking clearly.
Since PE symptoms can resemble other conditions, such as pneumonia or a heart attack, it is crucial for patients to recognize when symptoms are worsening. Recognizing the symptoms early and getting medical care can improve the chances of survival and reduce complications.
Classifications
PE is classified based on how much it disrupts blood flow and affects the heart. Some cases cause mild symptoms, while others can be life-threatening.
Massive PE or High-Risk PE
Massive PE occurs when a large clot completely or nearly completely blocks a major artery in the lungs, severely reducing blood flow. This causes a sudden drop in blood pressure, making it difficult for the heart to pump blood effectively.
Stage 2: Pre-Afib
Your heart might start showing brief periods of irregular activity. You might feel occasional palpitations or a racing heart. These episodes are not yet diagnosed as Afib. Tests like an ECG might not catch these changes unless they happen during the test.
- Symptoms: Severe shortness of breath, chest pain, dizziness, fainting, or even cardiac arrest.
- Without immediate treatment, organ failure and death can occur within hours.
- 30-day mortality rate: Between 25% and 65%, depending on how quickly treatment is started and whether the heart has already been affected.
Submassive PE or Intermediate-Risk PE
Submassive PE is less severe than massive PE but still dangerous. The clot reduces blood flow enough to strain the heart, but blood pressure remains stable. Tests may show signs of heart stress, such as an increased heart rate, reduced oxygen levels, or changes in heart function.
- Symptoms: Shortness of breath and chest discomfort, and in some cases, patients may show signs of right heart strain, which can lead to complications if untreated.
- 30-day mortality rate: 5% to 25%, depending on factors such as heart strain and overall health.
Low-Risk PE
Low-risk PE involves smaller clots that do not significantly affect blood flow or heart function. Blood pressure remains stable, and symptoms are usually mild.
- Symptoms: Mild shortness of breath and chest discomfort.
- 30-day mortality rate: Less than 1%, making it the least life-threatening classification.
Causes
PE occurs when a blood clot blocks blood flow in the lungs. These clots often originate from deep veins in the legs and travel through the bloodstream until they lodge in the lungs. This blockage prevents oxygen from reaching the body properly, leading to breathing problems, chest pain, and other complications.
Major Causes
- Sluggish Blood Flow: This can happen during long periods of inactivity, such as long flights, hospital stays, or recovery from surgery. When blood is not moving as it should, it becomes more likely to clot.
- Damage to Blood Vessels: Injuries, surgical procedures, or certain medical conditions can weaken veins. As the body attempts to repair the damage, it may form a clot that grows too large or breaks off, leading to PE.
- Underlying Conditions: Some patients are more prone to clotting due to inherited blood disorders, hormone-related changes (such as pregnancy or birth control use), and diseases like cancer. These conditions can make blood thicker or cause it to clot more easily, even without a clear trigger.
Less Common Causes
- Air Bubbles and Fat: In rare cases, PE can result from air bubbles or fat from broken bones entering the bloodstream and blocking blood flow in the lungs.
Diagnosis
If a PE is suspected, doctors may use a combination of imaging tests and lab work to confirm or rule out the condition.
Imaging Tests
- CT scan of the chest: This is the most common imaging test used to diagnose PE. It provides detailed pictures of your lungs and blood vessels to see if a blood clot is blocking blood flow. A special dye is injected into your vein before the scan to make the blood vessels show up more clearly.
- Ventilation-perfusion (V/Q) scan: This test is often used when a CT scan cannot be performed, for example, in patients with kidney disease or an allergy to the contrast dye used in CT scans. It measures how well air and blood are moving through different areas of your lungs.
Lab Tests
Blood tests alone cannot diagnose PE, but they can provide valuable information to help guide the next steps in testing.
- D-dimer Test: This blood test measures levels of a substance released when blood clots break down. If the D-dimer level is normal, PE is unlikely, and further testing may not be needed. However, if it is high, additional tests are required to confirm PE.
- Other Blood Tests: Some blood work may be done to check kidney and liver function, oxygen levels, and blood clotting status, especially in patients who have risk factors for PE.
Electrocardiogram (EKG)
Although an EKG cannot detect PE directly, it is often done to check the heart’s electrical activity. Some PE cases can put a strain on the heart, causing abnormal heart rhythms or changes in the EKG pattern. Since PE symptoms can resemble a heart attack, an EKG helps doctors rule out heart-related causes of chest pain.
Complications
Sudden Death
The most dangerous complication is sudden death. About 1 in 4 patients never realize they have a PE before it becomes fatal. When a large clot completely blocks a major artery in the lungs, blood flow stops, oxygen levels plummet, and within minutes, the heart and organs begin to shut down.
Heart Strain
Even when PE is not immediately fatal, it can put serious strain on the heart. The right side of the heart, which pumps blood to the lungs, must work much harder to push blood past the blockage. Over time, this extra effort can lead to right heart failure, where the heart weakens and struggles to keep up.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
Some patients develop long-term high blood pressure in the lungs, known as CTEPH. Instead of dissolving completely, the clot leaves scarring that narrows the lung’s arteries, making it harder for blood to circulate. This leads to persistent shortness of breath, fatigue, and an increased risk of heart problems.
Oxygen Loss
Oxygen loss is another major concern. Since PE reduces the amount of oxygen in the bloodstream, organs including the brain, kidneys, and liver may suffer damage, especially if blood flow is restricted for too long. Some patients experience confusion or weakness due to low oxygen levels, while others struggle with long-term complications even after the clot is gone.
Long-Term Effects
For many, PE is not just a single event but a lasting condition. Some continue to feel short of breath, fatigued, or experience chest discomfort long after treatment. While PE can often be treated successfully, the risks do not always go away once the clot is gone. The impact on the heart, lungs, and oxygen levels can have lasting consequences, especially in those with repeated episodes or underlying health conditions.
Treatment
The main goals of pulmonary embolism (PE) treatment are to:
- Prevent the existing blood clot from getting larger.
- Reduce your risk of developing new blood clots.
- Break up the blockage in severe cases.
The choice of treatment depends on the severity of the PE, overall health, and the risk of recurrence.
Anticoagulation Therapy (Blood Thinners)—Standard Treatment
Anticoagulants are the primary treatment for most cases of PE. These medications prevent existing clots from getting larger and reduce the risk of new clots forming.
- Direct-Acting Oral Anticoagulants (DOACs): These are now considered the first-line and preferred treatment for PE due to their effectiveness and convenience. Medications such as rivaroxaban and apixaban work quickly and do not require frequent blood monitoring.
- Heparin: A fast-acting anticoagulant given by injection or IV, commonly used in hospital settings at the start of treatment.
- Lovenox (enoxaparin): Administered by injection, often used in specific cases such as pregnancy, or temporarily before switching to warfarin.
- Warfarin(anticoagulants): An older oral anticoagulant that requires regular blood monitoring but remains an option for patients who cannot take DOACs.
Most patients require blood thinners for at least 3 months. Long-term anticoagulation may be necessary for those with ongoing clotting risk or a history of multiple PEs.
Advanced Treatment for High-Risk PE
Patients with massive PE or severe right heart strain may require urgent intervention beyond anticoagulation.
- Fibrinolytic: Strong clot-breaking medications administered intravenously in life-threatening cases. They have a high risk of severe bleeding.
- Percutaneous Thrombectomy: A catheter-based procedure used to remove the clot, break it apart, or dissolve it with clot-busting medication. Considered for patients with large PE who are not candidates for fibrinolytics.
- Vena Cava Filter: A small metal filter placed in the vena cava, the large vein that carries blood back to the heart, to prevent clots from reaching the lungs. Used in patients who cannot safely take blood thinners.
The choice of treatment is based on individual patient risk factors, clot severity, and overall health condition. Early intervention improves outcomes and reduces complications.
Prevention
While not every case of PE can be avoided, your risk can often be reduced, especially if you have known risk factors. Staying active, maintaining good circulation, and following medical advice are important in preventing blood clots that could lead to PE.
For Patients Recovering from Surgery, Illness, or Prolonged Bed Rest
Doctors may prescribe blood thinners or compression stockings to improve circulation. Moving regularly, even after a short period of immobility, can also help keep blood flowing properly. Those on long flights or car rides should take breaks to stretch their legs and stay hydrated.
Personal or Family History of Blood Clots
If you have a personal or family history of blood clots, are pregnant, or take medications that affect clotting, speak with your doctor about your risk and whether preventive measures are needed.
Early Detection
Get medical help if you experience unexplained shortness of breath, chest pain, or swelling in one leg, as these could be early signs of a blood clot. Early detection and treatment can significantly lower your risk of serious complications.
Related Topics
All About Clotting Disorders
Blood clotting is a vital process that helps prevent excessive bleeding when we get injured. However, sometimes this blood clotting occurs when and/or where it isn’t supposed to. Other times, the clot forms properly, but then does not dissolve when it should.
Blood Thinners Don’t Really “Thin” Blood
Blood thinners, also known as anticoagulants, are medications that help prevent the formation of blood clots. They are commonly used to treat conditions involving the risk of blood clots, such as deep vein thrombosis (DVT), pulmonary embolism, atrial fibrillation, and certain heart conditions.
Which DOAC Is Best for You
DOACs are a newer type of blood thinners that prevent blood clots and treat conditions like deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as to prevent stroke in people with atrial fibrillation.
