- Atrial fibrillation (Afib) is an irregular and often rapid heart rhythm caused by disorganized electrical signals in the upper heart chambers (atria).
- Afib itself is not immediately life-threatening, it increases the risk of serious complications like stroke.
- Common symptoms: Racing, fluttering, or skipping heartbeats (palpitations), shortness of breath, fatigue, dizziness. However, some people feel nothing.
- Risk factors: Age, high blood pressure, heart disease, obesity, thyroid issues, alcohol, smoking.
- Treatment
- Medications: Heart rate control, heart rhythm control, blood thinners.
- Nonsurgical Procedures: Electrical cardioversion, catheter ablation, permanent pacemaker.
- Surgical Procedures: Maze procedure, left atrial appendage removal.
Overview
Atrial fibrillation, commonly called Afib, is a heart condition characterized by an irregular and often rapid heartbeat.
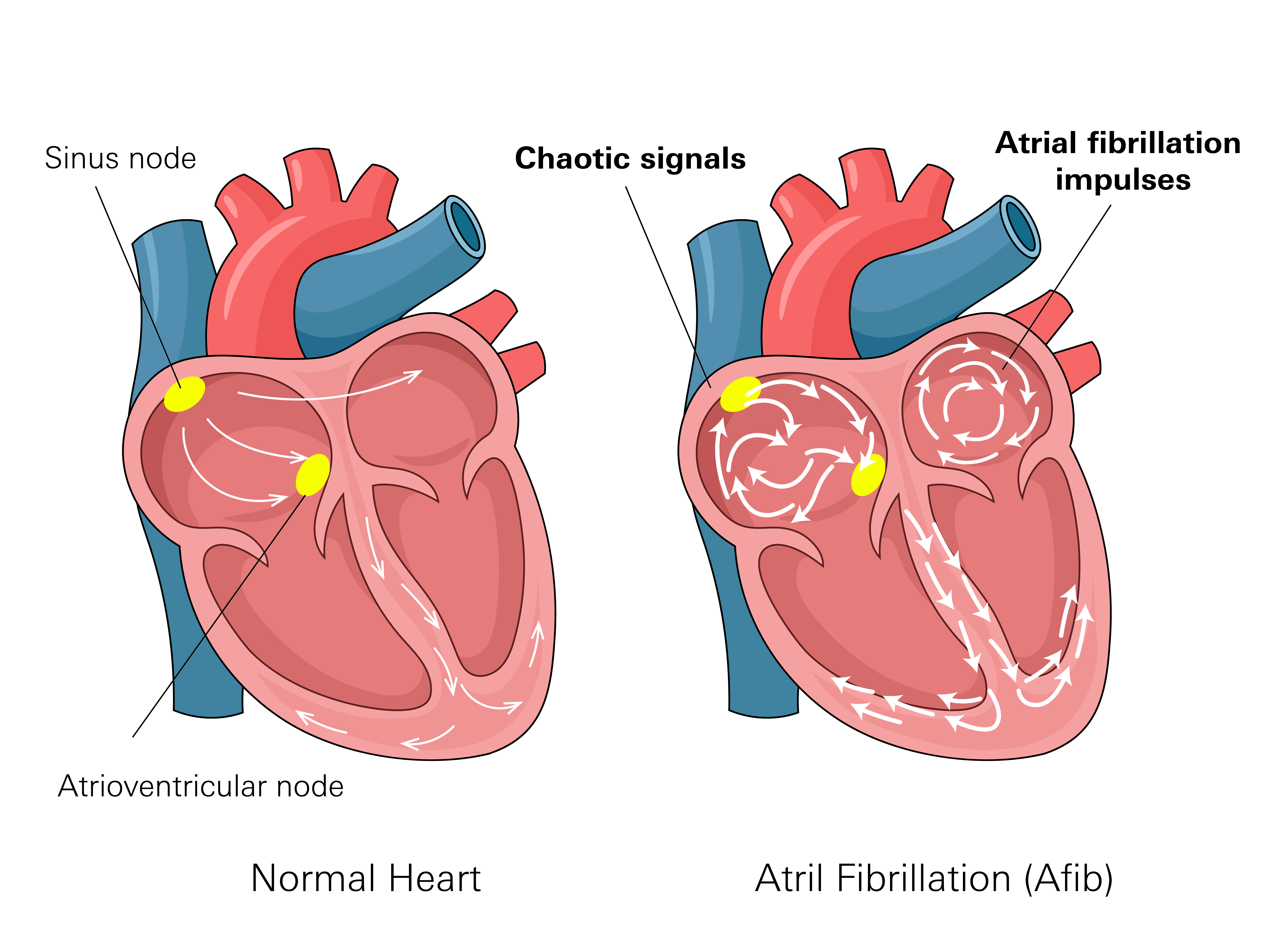
In a healthy heart, the atria (upper chambers) and ventricles (lower chambers) contract in a coordinated rhythm. This synchronized action efficiently pumps blood throughout the body. This rhythm originates from precise electrical signals that follow a specific pathway within the heart.
In Afib, these electrical signals become disorganized. Instead of sending steady signals that allow the atria and ventricles to work together, the atria begin to quiver or beat too fast. This disrupts the heart's normal rhythm, causing it to beat irregularly and sometimes at a much higher rate than usual. Since the atria are not contracting properly, blood does not flow efficiently into the ventricles, resulting in less effective blood pumping.
Afib can occur in short episodes that come and go, or it can be persistent, requiring medical treatment to help control the heart’s rhythm.
While Afib itself is not immediately life-threatening, it elevates the risk of serious complications if not treated. The inefficient pumping of blood can cause blood to slow down and pool, particularly in the atria. This stagnant blood can lead to the formation of blood clots. If these clots dislodge and travel through the bloodstream, they can obstruct blood flow to vital organs, potentially causing severe medical events.
Prevalence
Atrial fibrillation (Afib) is one of the most common heart rhythm disorders in the United States. Approximately 4% of adults have Afib, equating to about 10.55 million Americans.
Age is a major factor in the prevalence of Afib. It is uncommon in younger adults; studies indicate that only around 0.26% of individuals under 50 have this condition.
However, the incidence of Afib increases substantially with age. By age 90 and older, nearly 25% of individuals have Afib. This is partly due to natural age-related changes in the heart's electrical system and a higher incidence of other medical conditions that can contribute to irregular heart rhythms.
Gender also affects the risk of developing Afib. Studies show that men are diagnosed with Afib more often than women, making up about 55% of cases.
However, women make up a larger percentage of Afib cases in older age groups. After the age of 75, around 60% of patients with Afib are women. This shift occurs partly because women tend to live longer than men, meaning more of them reach the ages where Afib is most common.
Symptoms
Common Symptoms
Many Afib patients experience symptoms related to an irregular heartbeat and its effect on blood flow. These symptoms can come and go or be persistent.
- Irregular or rapid heartbeat: Your heart may feel like it is racing, fluttering, or skipping beats. This sensation is often described as palpitations.
- Shortness of breath: Some patients find it harder to breathe, especially during physical activity or when lying down.
- Fatigue: Your heart is not pumping blood as efficiently as it should, which can leave patients feeling unusually tired or drained.
- Dizziness or lightheadedness: Poor blood circulation can lead to feelings of faintness or unsteadiness.
- Chest discomfort: Some patients may feel pressure, tightness, or mild pain in their chest, though this is not always present.
Serious Symptoms
In some cases, Afib can lead to complications that require immediate medical attention. These symptoms may indicate that your heart is struggling to function properly or that a blood clot has formed.
- Severe chest pain: A sudden or intense pain in your chest may be a sign of a heart attack, especially if it is accompanied by sweating, nausea, or pain spreading to your arms, neck, or jaw.
- Fainting: A sudden loss of consciousness or feeling as if you might pass out can indicate that your heart is not supplying enough blood to your brain.
- Weakness on one side of your body or difficulty speaking: These may be signs of a stroke, which can occur if a blood clot forms in your heart and travels to your brain.
- Severe shortness of breath: If breathing becomes difficult even while at rest, it may indicate that your heart is not pumping enough blood to supply your body with oxygen.
Stages
Afib progresses through different stages based on how often it occurs and how it affects the heart over time.
Stage 1: At Risk for Afib
You don't have Afib yet, but things like high blood pressure, obesity, sleep apnea, diabetes, or heart disease make it more likely to develop. You probably won't feel anything unusual. Managing these risk factors might help prevent Afib.
Stage 2: Pre-Afib
Your heart might start showing brief periods of irregular activity. You might feel occasional palpitations or a racing heart. These episodes are not yet diagnosed as Afib. Tests like an ECG might not catch these changes unless they happen during the test.
Stage 3: Diagnosed Afib
You have been diagnosed with Afib. This stage has different types based on how often it happens:
- First-detected Afib: This is the first time Afib is found. It might not happen again.
- Paroxysmal Afib: Afib comes and goes, lasting from minutes to days and then stopping on its own.
- Persistent Afib: Afib lasts longer than 7 days and needs medical treatment to go back to a normal rhythm.
- Long-standing persistent Afib: You've had Afib for over a year, even with attempts to fix it. Your heart might have changed, making it harder to get a normal rhythm back.
People can move between these types of Afib. Sometimes it happens more often, sometimes less.
Stage 4: Permanent Afib
Afib is constant and can't be fixed with treatment. The goal now is to manage symptoms and prevent problems like stroke or heart failure. Doctors will likely prescribe medications to control your heart rate and blood thinners. Permanent Afib means the focus is on keeping your heart as healthy as possible, not on trying to restore a normal rhythm.
Causes
Heart-related conditions
- High Blood Pressure: Extra strain on the heart can lead to structural changes.
- Coronary artery disease: Narrowed or blocked arteries reduce blood flow to the heart.
- Heart failure: A weak or stiff heart struggles to pump blood efficiently.
- Heart valve disease: Abnormal valves disrupt normal blood flow, triggering irregular heartbeats.
- Previous heart attack Long-term stress can raise blood pressure and may lead to unhealthy behaviors like smoking or overeating, indirectly increasing the risk of CAD.
- Family History: Damaged heart tissue can interfere with electrical signals.
Other conditions
- Overactive thyroid (hyperthyroidism): Excess thyroid hormone can speed up the heart rate.
- Obesity: Extra weight increases strain on the heart and contributes to other risk factors.
- Diabetese: High blood sugar levels can damage blood vessels and affect heart function.
Lifestyle factors
- Excess alcohol: Drinking heavily can trigger Afib episodes.
- Caffeine and stimulants: These can cause fast or irregular heartbeats in some people.
- Smoking: Damages blood vessels and increases the risk of heart disease.
- High stress: Can raise heart rate and trigger irregular rhythms.
Age and genetics
- Aging: The risk of Afib increases after age 60 as the heart’s electrical system changes.
- Family history: Those with close relatives who have Afib may be more likely to develop it.
Some patients may develop Afib due to a combination of these factors, while others may experience it without an obvious cause.
Diagnosis
If you have symptoms that could be Afib, your doctor will start by reviewing your health history and giving you a physical exam, such as checking your heart rate, asking about palpitations, shortness of breath, and dizziness. Because Afib doesn't always happen all the time, more tests are often needed to confirm it and see how often it occurs.
Electrocardiogram (ECG)
An ECG records your heart’s electrical signals. Small electrodes are placed on your chest, arms, and legs to capture a brief snapshot of heart activity. This test can detect irregular rhythms, but since Afib can come and go, it may not always appear on a single ECG recording. If the results are normal but Afib is still suspected, longer-term monitoring may be recommended.
Heart Rhythm Monitoring
For patients whose Afib is not detected on a standard ECG, wearable heart monitors can track electrical activity over an extended period. These include:
- Holter monitor: A small, portable device worn for 24 to 48 hours that continuously records heart activity. It helps capture irregular rhythms that may not have been seen during a short ECG test.
- Event monitor: Similar to a Holter monitor but used for a longer period, usually 2 to 4 weeks. This device records heart activity when an irregular rhythm is detected or when you activate it after experiencing symptoms.
- Implantable monitor: A small device placed under your skin that continuously tracks heart rhythms for months or longer. It is used when Afib episodes are rare but still suspected.
Echocardiogram
An echocardiogram is an ultrasound test that provides moving images of your heart. It helps healthcare providers evaluate the size and function of the heart chambers, as well as detect structural issues or blood clots that may be associated with Afib.
Stress Test
A stress test measures how your heart responds to physical activity. It is performed either while walking on a treadmill or using medication that stimulates your heart in a similar way. This test helps determine if underlying heart conditions, such as poor blood flow to your heart muscle, are contributing to Afib.
Treatment
Treatment focuses on managing your heart’s rhythm, controlling heart rate, and reducing the risk of complications such as stroke. Some options involve medications, while others include procedures that help restore or maintain a normal heartbeat.
Medications
Medications are often the first approach used to manage Afib. These can help control heart rate, stabilize heart rhythm, or prevent blood clots.
- Heart rate control: Beta-blockers, calcium channel blockers, and digoxin help slow your heart down so it does not beat too fast.
- Heart rhythm control: Antiarrhythmics, including amiodarone, help keep your heart beating in a normal rhythm.
- Blood thinners(anticoagulants): Since Afib increases the risk of blood clots, blood thinners are often prescribed to lower the risk of stroke. These include warfarin, apixaban, dabigatran, edoxaban, and rivaroxaban.
Nonsurgical Procedures
For patients who do not respond well to medications or need additional treatment, certain minimally invasive procedures can help restore or maintain a normal heart rhythm.
- Electrical cardioversion: This procedure uses low-energy electrical shocks to reset your heart’s rhythm. Cardioversion is often a short-term solution and may need to be repeated or followed by other treatments to maintain a normal rhythm.
- Catheter ablation: Thin tubes or catheters are inserted into blood vessels and guided to your heart. Radiofrequency energy is then used to destroy small areas of tissue responsible for the irregular rhythm.
- Permanent pacemaker: In cases where the heart beats too slowly, a small device is implanted near the heart to send electrical impulses that regulate the heartbeat.
Medical Procedures
Surgery is usually considered when medications and less invasive procedures haven't worked, or if a patient is already having heart surgery for another reason.
- Maze procedure: A surgeon creates a pattern of scar tissue in your heart using a scalpel or laser. Since scar tissue does not conduct electrical signals, this helps prevent irregular rhythms.
- Left atrial appendage removal: If blood clots are a concern, the left atrial appendage may be removed during surgery to lower the risk of stroke.
Prevention
While not all cases of Afib can be prevented, certain lifestyle choices and management can help lower the risk of developing this condition. Reducing strain on the heart and maintaining overall heart health play an important role in prevention.
If you experience symptoms such as a fluttering heartbeat, dizziness, shortness of breath, or unexplained fatigue, it is important to talk to your doctor. Since Afib can increase the risk of complications like stroke, early detection is crucial.
When speaking to your doctor, consider the following:
- Describe any symptoms, including when they started and how often they occur.
- Mention any medical conditions or medications being taken.
- Ask about testing options to check for irregular heart rhythms.
- Discuss ways to reduce personal risk factors and maintain heart health.
Although Afib can be a long-term condition, managing it properly can help improve quality of life and reduce complications. Regular follow-ups and monitoring can help track heart health over time and determine if treatment adjustments are needed.
Related Topics
The Link Between Atrial Fibrillation and Stroke
In AF, the atria do not contract effectively, which can lead to the formation of blood clots. If a blood clot forms in the atria, it can travel to the brain and block blood flow to a part of the brain, causing a stroke.
Five Most Common Arrhythmias
There are several types of arrhythmias, and they can be categorized based on their origin and the speed of heartbeats.
The Most Dangerous Arrhythmia: Ventricular Fibrillation
Ventricular fibrillation, or “V fib” is considered the most dangerous type of arrythmia. Instead of squeezing and pumping blood to the lungs and body, the ventricles just quiver and flutter in a rapid, uncoordinated, and chaotic manner.

