- Raynaud's syndrome affects blood flow to extremities (fingers and toes). It causes blood vessels to narrow more than usual, leading to color changes, numbness, and discomfort.
- About 4.85% of U.S. adults experience Raynaud's symptoms. It is more common in women and typically affects younger adults, especially under 40.
- Episodes often involve skin color changes (white, blue, red), coldness, numbness, tingling, and pain. Episodes can last from a few minutes to an hour and are triggered by cold or stress.
- There are two types: primary (occurs alone, less severe) and secondary (linked to other conditions, more serious). Secondary Raynaud's is often associated with autoimmune diseases.
- Risk factors include age, sex, climate, family history, autoimmune diseases, certain jobs, smoking, and some medications.
- Treatment focuses on lifestyle changes (staying warm, managing stress, quitting smoking) and medications (calcium channel blockers, PDE5 inhibitors). Severe cases may require procedures like Botox injections or surgery.
Overview
Raynaud's condition, also known as Raynaud's phenomenon or disease, impacts blood flow to extremities such as fingers and toes, and sometimes the nose, ears, or lips. The small blood vessels that supply blood to the skin become much narrower than normal, which reduces blood flow to the affected areas.

Consequently, the skin may change color to white or blue, and become uncomfortable. As blood flow returns, the area can turn red and feel warm or throb. These color changes are a key indicator. Other symptoms include tingling, aching pain, stiffness, a burning sensation, or skin tightness. Episodes typically last from a few minutes to an hour.
Raynaud's is more prevalent in women and often begins before age 40. Many patients are unaware they have the condition, as symptoms can be mild or come and go.
There are two main types: primary and secondary Raynaud's. Primary Raynaud's is more common, appears on its own, and is generally less severe. Secondary Raynaud's is less common but more serious; it happens as part of another medical condition, often autoimmune diseases. Secondary Raynaud's can involve damage to blood vessels, increasing the risk of complications like sores.
Common triggers for episodes include cold temperatures and emotional stress. Even simple things like holding a cold drink or walking into a chilly room can cause a reaction.
Prevalence
Around 4.85% of U.S. adults report symptoms consistent with Raynaud’s. This means nearly 1 in 20 adults may experience these blood vessel spasms, often without knowing the condition's name.
Raynaud’s is more common in women than men and is frequently reported in younger age groups, especially those under 40. However, it can affect adults across various climates and geographic regions.
Studies also show that people in colder regions are more likely to report symptoms, as cold temperatures are a common trigger, making episodes more frequent and noticeable. This may explain why it is sometimes diagnosed more often in northern states compared to warmer southern areas.
It's important to note that Raynaud's often goes undiagnosed. Many people consider their fingers turning pale, blue, or numb in the cold as a normal reaction. Since episodes are often intermittent and may not cause lasting pain or injury, individuals might not mention them to their doctor. Therefore, the actual number of people with Raynaud's may be higher than current estimates.
Symptoms
Raynaud’s syndrome tends to follow a pattern. What patients usually notice first is a change in skin color, often in the fingers or toes, though sometimes the nose, lips, or ears can be involved too.
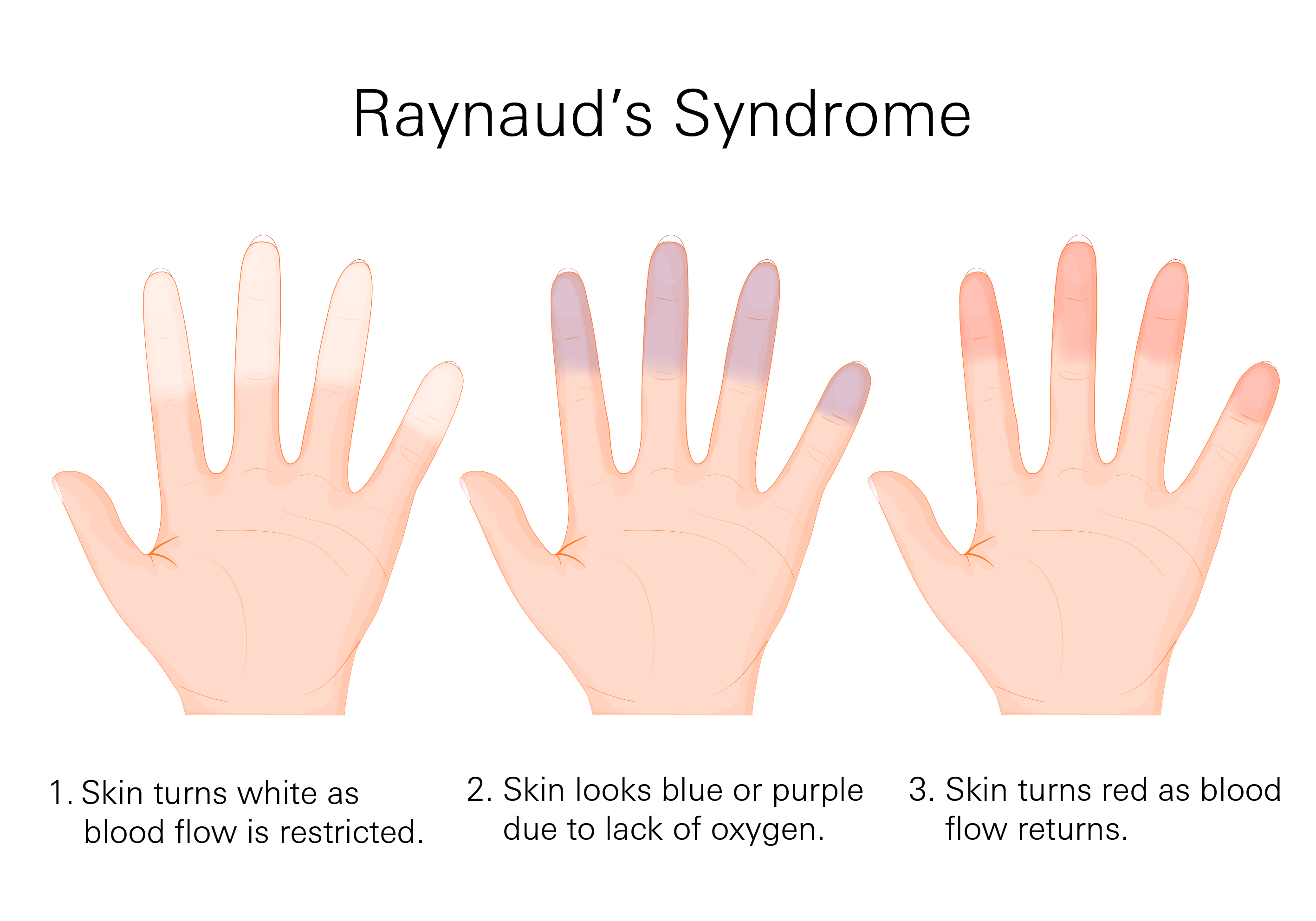
A typical episode may unfold in 3 phases:
- Pale or white: The area turns white due to a sudden drop in blood flow.
- Blue or purple: As blood flow remains restricted, the skin can start to look blue or purple because of the lack of oxygen.
- Red: When blood returns, the area might turn bright red and feel warm or throbbing.
These color changes do not always happen in this exact order or in all three stages. Some patients might only notice the white and red phases, or feel coldness and tingling without much color change. However, color changes are the most recognizable sign.
During an episode, you may also notice:
- Coldness or numbness in the fingers or toes
- Tingling or a pins-and-needles feeling
- Throbbing or aching pain as blood flow returns
- Stiffness or difficulty moving the fingers
- A burning sensation once the episode passes
- Skin tightness or discomfort, especially during longer episodes
Most episodes last a few minutes to an hour and are often triggered by exposure to cold (even something as simple as holding a cold drink) or emotional stress.
When Should You Be Concerned?
If you’re experiencing any of the following, it’s worth bringing up with a doctor:
- Episodes that happen frequently or last longer than 20-30 minutes
- Fingers or toes that stay discolored even after warming up
- Pain that lingers well after the episode ends
- Sores, cracks, or ulcers on the tips of your fingers or toes
- Thickened, shiny, or tight skin around the fingers
- Nails that are changing shape or texture
- One hand or foot is always affected more than the other
- Sudden onset of symptoms after age 40
- A history of autoimmune conditions or symptoms such as joint pain, muscle weakness, or fatigue that appear along with Raynaud’s episodes
Even if your symptoms seem mild, if they’re affecting your daily activities, such as making it hard to type, hold items, or be outside in cooler weather, it’s worth discussing with a provider.
Causes
Raynaud's syndrome has two main types, each with distinct characteristics and causes.
Primary Raynaud's
- This type is more common and occurs on its own, not linked to other diseases.
- It happens when the nerves controlling blood flow are overly sensitive. Small changes in temperature or stress can trigger a strong reaction, causing blood vessels to narrow excessively.
- There is no clear damage to the blood vessels; they just react too forcefully.
- Typically begins in younger adults, between ages 15 and 30.
- Generally less severe, with many patients not developing other health issues. However, it can still cause discomfort, especially in cold environments or stressful situations.
Secondary Raynaud's
- This type is less common but more serious, occurring as part of another medical condition.
- Often associated with autoimmune conditions like scleroderma, lupus, or rheumatoid arthritis. These diseases cause the body to attack its own tissues, affecting blood vessels.
- Blood vessels may become damaged or stiffened, making episodes more intense.
- Higher risk of complications, such as sores or ulcers on the fingertips if blood supply is restricted for too long.
- Tends to appear later in life and may come on suddenly. Severe symptoms or onset after age 40 may require further testing.
Common Triggers
Both types of Raynaud's can be triggered by similar factors:
- Cold Temperatures: Most common triggers. Handling cold objects, walking into a chilly room, or cold weather can cause symptoms.
- Emotional Stress: Stressful situations can also trigger episodes.
Risk Factors
Raynaud's syndrome does not affect everyone equally. Several factors may increase the likelihood of developing the condition.
Age and Sex
Primary Raynaud's is more likely to start between the ages of 15 and 30. It also occurs more often in women than in men. The exact reasons are not fully understood, but hormonal factors may play a role.
Climate
Living in a colder climate can increase the risk of being diagnosed with Raynaud's or experiencing more symptoms. While cold weather doesn't cause Raynaud's, it can easily trigger episodes.
Family History
Having a family member, especially a parent or sibling, with Raynaud's increases your risk of developing it, particularly primary Raynaud's. H
Autoimmune or Connective Tissue Diseases
Secondary Raynaud's is often associated with autoimmune conditions. These include:
- Scleroderma
- Lupus
- Rheumatoid arthritis
- Sjögren’s syndrome
Smoking
Smoking affects blood vessels and can reduce blood flow to the skin. This narrowing effect can increase the risk of vasospasm and lead to more frequent or intense episodes. Smokers with Raynaud’s may also have a higher risk of complications over time. See tips on how to quit smoking.
Medications
Some medications can trigger or worsen Raynaud’s symptoms, including:
- Beta blockers
- Migraine medications containing ergotamine
- Certain chemotherapy drugs
- Stimulants, including methylphenidate
- Decongestants, especially those with pseudoephedrine
Certain Jobs or Activities
Repeated trauma to the hands, even from routine tasks, may elevate the risk of developing Raynaud's.
Diagnosis
Initial Conversation
Your provider will likely ask about:
- What happens during an episode (e.g., how your fingers look and feel)
- Duration of symptoms
- Triggers (cold, stress, medications)
- Family history of similar symptoms
- Other health changes (joint pain, skin thickening, fatigue)
Physical Exam
Your provider may perform a physical exam, focusing on your hands, fingers, toes, and nails. They’ll look for signs of skin changes, ulcers, thickening, or other features that might indicate a more complex cause.
Tests to Determine Type
- Nailfold Capillaroscopy: This non-invasive test involves using a microscope or magnifying tool to examine the tiny blood vessels (capillaries) at the base of your fingernails (the nailfold).
- Primary Raynaud's: Capillaries usually appear normal, possibly fewer in number or less defined.
- Secondary Raynaud's: Capillaries may be widened, twisted, irregular, and may show signs of bleeding or damage. These patterns can indicate an underlying connective tissue disease.
- Blood Tests: To check for markers of inflammation or autoimmunity if there’s concern about an autoimmune condition.
- Primary Raynaud's: Capillaries usually appear normal, possibly fewer in number or less defined.
Blood tests do not diagnose Raynaud’s by themselves but help doctors determine if something else may be contributing to your symptoms. If blood work is normal and nailfold capillaries look typical, it points toward primary Raynaud’s.
In some cases, doctors may also check thyroid function, as thyroid disorders can sometimes mimic or worsen Raynaud’s symptoms.
Treatment
’s syndrome does not have a cure, but there are several ways to manage symptoms. Treatment focuses on two main goals: reducing the number of episodes and protecting affected areas from damage.
Lifestyle Changes
- Stay Warm
- Avoid Sudden Temperature Changes
- Manage Stress
- Quit Smoking
For many patients with mild symptoms, these lifestyle changes are enough to keep Raynaud’s manageable. However, if episodes continue to occur frequently or start affecting daily activities, medication may be needed.
Medications
When medication is necessary, the first choice is usually calcium channel blockers. These medications help blood vessels relax and stay open longer, improving blood flow to the fingers and toes.
- Nifedipine: The most commonly used calcium channel blocker for Raynaud’s.
- Studies show calcium channel blockers can reduce the number of Raynaud’s episodes by about three per week on average and make each episode shorter and less painful.
If calcium channel blockers are not effective or cause intolerable side effects, doctors may recommend other medications:
- Phosphodiesterase Type 5 (PDE5) Inhibitors: Medications like sildenafil or tadalafil improve blood flow and widen blood vessels in the fingers and toes.
- Prostanoids: Strong vasodilators like iloprost, given through a vein in severe cases, especially when ulcers or sores develop.
- Endothelin Receptor Antagonists: Medications like bosentan used when Raynaud’s causes difficult-to-heal ulcers.
- Angiotensin Receptor Blockers: Medications like losartan sometimes used for Raynaud’s.
Common side effects of these medications include low blood pressure, dizziness, headaches, and leg swelling. Doctors usually start with a low dose and adjust it based on your response.
Procedures for Severe Cases
If medications are not enough, certain procedures may be considered for serious complications, such as non-healing ulcers or signs of permanent damage:
- Botox Injections: Used to relax blood vessels and improve blood flow.
- Digital Periarterial Sympathectomy: A surgical procedure where small nerves near blood vessels are cut to reduce constriction leading to Raynaud’s attacks. This is generally considered when all other options have been tried.
These procedures are not commonly used, and research is ongoing to understand their long-term effectiveness.
When Raynaud’s Becomes an Emergency
Raynaud’s episodes are usually uncomfortable but temporary. However, a rare but serious complication called acute digital ischemia can occur when blood flow is cut off for a long time, similar to a heart attack but in a finger or toe.
Signs of acute digital ischemia include:
- A finger or toe that stays white, blue, or purple for more than 45 minutes
- Severe pain and tenderness that does not improve
- Skin starting to break down or show open sores
If you experience these symptoms, it is a medical emergency. Immediate treatment in a hospital may be needed to restore blood flow and prevent permanent damage.
Prevention
While Raynaud’s syndrome cannot be completely avoided, there are ways to reduce the number and severity of episodes. The most important part is keeping your body warm, not just your hands and feet, but your entire body. Dressing in layers, wearing a hat, and protecting your chest and core can help keep blood vessels stable.
Avoiding sudden temperature changes, managing stress, and quitting smoking are also important. These habits help prevent the blood vessels from tightening unnecessarily.
Gentle exercise, such as walking or swimming, can improve circulation overall. Using moisturizers regularly helps protect your skin from cracking, especially during cold weather.
Prevention focuses on protecting blood flow, reducing triggers, and avoiding damage to the fingers and toes. Small daily habits can go a long way in keeping symptoms under better control.
Related Topics
Calcium Channel Blockers and High Blood Pressure
Calcium channel blockers, also known as calcium channel antagonists, are frequently prescribed to lower blood pressure.
Losartan: Insights and Benefits
Losartan (pronunciation: low·saar·tn) is used for treating hypertension (high blood pressure). It also helps to protect the kidneys from damage due to diabetes.
Buerger's Disease
Buerger's disease is a rare condition affecting the blood vessels of the arms and legs. It causes inflammation in the small and medium-sized arteries and veins, primarily in the hands and feet.
